The most common forms of Charcot Marie Tooth disease
Charcot Marie Toot's disease belongs to the category of hereditary neuropathies , which are characterized by damage to the fibers of the peripheral nervous system, both sensory and motor.
You can often find other names for the pathology. For example, peroneal or neural amyotrophy of Charcot-Marie. This nosology is considered one of the most common representatives of hereditary diseases, as it occurs in 25-30 people per 100 thousand population.
In modern neurology, there are 4 variants of the disease . But most likely this is not the final number. After all, all types of mutations in genes that can lead to disease are still not known.
Charcot's syndrome of the first (or demyelinating) type is observed in 60% of patients. It debuts before the age of twenty, more often even in the first years of a child’s life. The disease is transmitted in an autosomal dominant manner. The second variant of the pathology, also called axonal and occurring in 20% of cases , is inherited in the same way. That is, when one of the parents is sick, the children will in any case “get” this genetic “damage” and it will then develop into a disease. But in the latter type of amyotrophy, the manifestation of symptoms is sometimes delayed until 60-70 years.
The two types of Charcot Marie Tooth disease differ in that the first involves destruction of the myelin sheath of the nerve, while the second primarily damages the axon.
The third variant of the pathology is the one that is inherited dominantly through the X chromosome. However, in men the symptoms are more pronounced than in women. What will make a doctor think about this version of the syndrome is the information that signs of the disease are not found in men in every generation of the family.
Neural amyotrophy type 4 is considered demyelinating and is inherited autosomal recessively , that is, there is a chance of having healthy children from sick parents.
Risk factors and causes of CMT
CMT is a hereditary disease, so people who have close relatives with the disease have a higher risk of developing the disease.
The disease affects peripheral nerves. Peripheral nerves are made up of two main parts: the axon, which is the inner part of the nerve, and the myelin sheath, which is the protective layer around the axon. CMT can affect the axon and myelin sheath.
At CMT 1
genes that cause the breakdown of the myelin sheath are mutated. Eventually, the axon is damaged and the patient's muscles no longer receive clear messages from the brain. This leads to muscle weakness and loss of sensation or numbness.
For CMT 2
the mutating gene directly affects axons. The signals are not transmitted strongly enough to activate the muscles and senses, so patients have weak muscles, poor sensation, or numbness.
ShMT 3
or
Dejerine-Sottas disease
, a rare type of disease. Damage to the myelin sheath leads to severe muscle weakness and soreness. Symptoms may be noticeable in children.
ShMT 4
is a rare disease that affects the myelin sheath. Symptoms usually begin in childhood and patients often require a wheelchair.
ShMT X
caused by a mutation on the X chromosome. It is more common in men. A woman with CMT X will have very mild symptoms.
What causes lead to the development of Charcot's disease?
The main and only cause of any type of Charcot-Marie-Tooth disease is point mutations in genes.
At the moment, science knows about two dozen genes that undergo changes that subsequently lead to amyotrophy. Most often, “breakdowns” are found in genes located on chromosomes 1 and 8, namely PMP22, MPZ, MFN2, etc. And this is only a part of them. Many remain behind the scenes, so to speak, because about 10-15% of patients do not even know about their illness and do not seek medical help.
The demyelinating type of pathology is also associated with acquired autoimmune aggression, in which the cells that create the outer sheath of the nerve are perceived by the body as foreign and are destroyed.
There are also risk factors that contribute to a more pronounced manifestation of the symptoms of Charcot-Marie-Tooth disease and aggravation of the existing clinical picture.
Triggers of the disease include:
- alcohol consumption;
- use of potentially neurotoxic drugs. For example, vincristine, lithium salts, metronidazole, nitrofurans, etc.
Anesthesia using thiopental is contraindicated for patients suffering from hereditary peroneal amyotrophy.
Physiotherapy
For Charcot-Marie-Tooth amyotrophy, the use of physiotherapeutic treatment methods is indicated. Massage, balneotherapy, electrical stimulation, mud therapy, therapeutic baths, and hydromassage are used.
For symptoms associated with impaired sensitivity, electrophoresis and galvanization are used with caution. If the sensory nerves are not affected, electrophoresis is performed with calcium and anticholinesterase preparations.
The main goals of physiotherapeutic treatment of Charcot-Marie-Tooth disease:
- activation of metabolism;
- reduction of dystrophy;
- improving blood circulation;
- activation of the conductivity of the neuromuscular system;
- normalization of psycho-emotional state.
How does Charcot-Marie-Tooth disease manifest?
Charcot-Marie-Tooth disease does not always manifest itself in the same way, even within the same family. And it’s not about the variety of its signs. The fact is that the genes encoding this pathology are capable of forming symptoms with varying degrees of severity. Simply put, having an identical “breakage” in the chromosomes, the signs of the disease in the father and son will have an individual coloring.
General symptoms
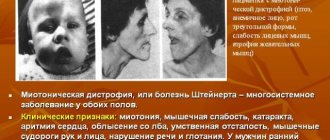
The clinical picture of the disease practically does not depend on its type and includes:
- atrophy of the muscles of the distal, that is, the most distant from the body, parts of the limbs;
- decreased tendon and periosteal reflexes;
- a change in sensitivity, characterized by its loss, but never accompanied by the appearance of a tingling or “crawling” sensation;
- deformation of the musculoskeletal system – scoliosis, enlarged arch of the foot, etc.
But still, there are a number of signs that slightly distinguish the course of the disease in its various variants.
First type
Charcot-Marie-Tooth disease of the first type often occurs in an exclusively erased form, in which patients do not feel changes in the body and do not seek medical help at all.
If the pathology manifests itself, then this happens during the first, maximum second, decade of life. In this case, the following are observed:
- painful cramps in the muscle mass of the lower leg, rarely in the calf muscle, more often in the anterior muscle group. Such spasms increase after a period of prolonged physical activity (walking, playing sports, cycling);
- changes in gait associated with a gradual increase in muscle weakness. Moreover, in children this may debut in tiptoeing;
- deformation of the feet with the formation of a high arch of the latter and the presence of hammertoes, which develops as a result of an imbalance in the tone of the flexors and extensors;
- muscle atrophy , starting from the feet and rising to the lower leg. Then the process affects the hand - tremors appear in the hands and severe weakness in the fingers, especially when trying to perform small movements. For example, fastening buttons, sorting cereals;
- depression or complete absence of tendon and periosteal reflexes , namely Achilles, carporadial, while the more proximal parts of the arms and legs are preserved. That is, the knee and reflexes from the biceps and triceps muscles remain intact;
- disturbances of sensitivity in the hands and feet , expressed in its gradual loss. Moreover, the pathology starts from the vibration and tactile sphere, spreading to joint-muscular and pain sensations;
- scoliosis and kyphoscoliosis;
- thickening of the nerve trunks, most often the superficial peroneal and greater auricular.
Charcot's disease is characterized by muscle atrophy in the distal limbs. Moreover, if subcutaneous fat is not expressed, the volume of the lower leg and thigh is strikingly different, and the legs take on the appearance of those of a stork or resemble an inverted champagne bottle.
Charcot-Marie neural amyotrophy type 1 has atypical forms. One of them is Rusi-Lewy syndrome , in which there is pronounced tremor when trying to hold the arms in one position and instability when walking. This also includes a disease that, in addition to standard symptoms, manifests itself as paresis, hypertrophy of the lower leg muscles, a sharp loss of sensitivity and night cramps in the calf muscles.
Second type
Charcot-Marie-Tooth disease of the second type, in addition to a later onset, is characterized by:
- less pronounced changes in sensitivity;
- less common occurrence of foot and toe deformities;
- the presence of restless legs syndrome (unpleasant sensations occur in the legs while going to bed, forcing the patient to move, which alleviates the condition);
- often preserved strength in the hand;
- absence of thickening of nerve trunks.
With Charcot-Marie-Tooth syndrome, transmitted through the X chromosome, sensorineural hearing loss (hearing loss) and transient encephalopathy that occurs after physical activity at altitude may occur. The latter is characterized by the appearance of symptoms 2-3 days after exercise. Signs of pathology include unsteadiness, difficulty speaking, swallowing, and weakness in the proximal parts of the arms and legs. Usually the clinical picture of the disease disappears on its own within a couple of weeks.
Kinds
The forms of the disease are distinguished taking into account the nature of damage to nerve endings belonging to the peripheral nervous system. Type 1 pathology develops due to demyelination - destruction of the myelin sheath covering the nerves. Normally, the myelin sheath improves the transmission of nerve impulses. It debuts more often in middle childhood (4-5 years), less often in adolescence.
The first symptoms: weakness in the feet, atrophic changes in the muscles of the distal legs. Atrophic changes in the muscle tissue of the hands develop later. Along with the loss of sensitivity (inability to distinguish temperature, perceive painful stimuli, vibration), a decrease (sometimes loss) of tendon reflexes is observed in the area of the hands and feet.
Charcot-Marie-Tooth polyneuropathy type 2 develops against the background of damage to axons - the branches of neurons through which communication is carried out between individual elements of the neuronal network. This is a slowly progressive form. Onset symptoms may appear in older children. During instrumental diagnostics, relatively normal indicators of the speed of nerve impulses are revealed.
In parallel, a decrease in the difference between the amplitude values of action potentials (excitation wave) of sensitive nerve cells is observed. Another feature is polyphasic (multiphasic) action potentials in the region of muscle fibers. A biopsy shows Wallerian-type axonal degeneration, the process of destruction of a section of an axon.
What is needed to confirm the diagnosis
It must be remembered that, first of all, the doctor will be able to suspect Charcot-Marie-Tooth disease if there is a burdened family history, that is, the presence of similar symptoms in one of the patient’s closest relatives.
Of the instrumental examination methods, the most informative is electroneuromyography (ENMG). In this case, a decrease in the speed of impulse transmission along the nerves is detected from normal 38 m/s to 20 m/s in the arms and 16 m/s in the legs. Sensory evoked potentials, which are not evoked at all or have a significantly reduced amplitude, are also examined.
In the second type of Charcot syndrome, changes in ENMG do not occur. Pathology is observed only when examining evoked sensory potentials.
A nerve biopsy with histological analysis of the obtained materials allows definitive confirmation of the presence of neural amyotrophy.
In this case, the first variant of the disease is characterized by:
- demyelination and remyelination of fibers with the formation of “onion heads”;
- decrease in the proportion of large myelinated fibers;
- axonal atrophy with a decrease in their diameter.
And the second type of Charcot Marie Tooth disease is not accompanied by demyelination and the formation of “bulb heads”, otherwise the signs are the same.
Diagnosis of the disease
The diagnosis is based on a study of the genetics of the patient and the characteristics of the manifestation of the disease. The doctor should carefully ask about the symptoms and history of the disease and examine the patient.
Nerve and muscle reflexes must be checked. For these purposes, EMG is used to record nerve conduction parameters.
A DNA test and a general blood test are prescribed. If necessary, a nerve fiber biopsy is performed.
A rare and very dangerous Tay-Sachs disease has a poor prognosis and is practically untreatable. Details in our article. A similar disease, Friedreich's hereditary ataxia, has similar symptoms and treatment approaches. What do you need to know about the disease?
Approaches to the treatment of Charcot's disease
At the moment, there is no specific therapy for Charcot's disease; only symptomatic therapy has been developed. Moreover, a greater emphasis is placed on exercise therapy and physical therapy. An equally important step is proper foot hygiene and wearing orthopedic shoes.
Surgery
Of the surgical interventions for Charcot's syndrome, arthrodesis of the ankle joints is most often used: removal of cartilaginous surfaces and fusion of the talus and tibia. This is accompanied by fixation of the leg in one position and loss of mobility of the foot, but allows you to maintain the ability to move.
Physiotherapeutic methods
When signs of pathology are identified, they immediately resort to teaching the patient exercise therapy exercises, which will allow maintaining the elasticity of muscles and tendons for as long as possible. Massage and aerobic exercise, for example, swimming and race walking, also have a beneficial effect on the condition of patients.
Main groups of drugs
The use of drugs for Charcot-Marie-Tooth disease is extremely limited due to their low effectiveness. For example, the use of vitamins, coenzyme Q, neuroprotectors and metabolites does not reduce the severity of pathological processes.
In cases where there is a sudden progression of symptoms and an increase in weakness in the legs, corticosteroids (Dexamethasone, Methylprednisolone), immunoglobulin preparations (Bioven mono) or plasmapheresis are prescribed. Since most often the cause of this deterioration is the addition of an autoimmune process.
A number of experiments have proven the positive effect of high doses of vitamin C on slowing down demyelination processes in type 1 Charcot disease.
If the patient complains of severe pain in the legs, then the drugs of choice are antidepressants (Amitriptyline) and anticonvulsants (Gabapentin, Lamotrigine, Topiramate).
Results
Charcot-Marie-Tooth disease is a hereditary neuropathy. It is widespread throughout the world, occurring in all races and ethnic groups. Although the disease was discovered by 3 doctors (Jean-Marie Charcot, Pierre Marie and Howard Henry Tooth) in 1886, the causes of some forms of the disease remain unclear.
Molecular genetics has to date identified causative mutations in 40 genes and has made a significant contribution to the molecular genetic classification of CMT and to the understanding of pathogenesis.
Inheritance includes all types of monogenic transmission - utosomal dominant, utosomal recessive, gonosomal dominant.
Since there is no cause-and-effect therapy, the current treatment strategy is based on rehabilitation, prosthetics and orthopedic treatment. The prognosis for patients with the vast majority of forms is favorable, since it does not reduce normal life expectancy, although it significantly affects its quality.
Forecast
Charcot-Marie-Tooth disease has a chronic progressive course, but the symptoms of the pathology develop extremely slowly - for years, or even decades. Patients are able to walk and care for themselves without assistance almost until the end of their lives. Of course, this is only possible if treatment measures are carried out in a timely manner and further recommendations of the doctor are followed.
Charcot's syndrome is not fatal. The life expectancy of patients is in no way related to the presence of this disease.
The patient’s condition can be aggravated by pregnancy, as well as the use of drugs prohibited for this pathology: Thiopental, Vincristine, etc. In 20-25% of cases, the deterioration is associated with the addition of an autoimmune process, in which cells, the purpose of which is to protect the body from foreign antigens, begin to attack the myelin the sheath of your own nerves.
It must be remembered that patients suffering from Charcot-Marie-Tooth disease need competent career guidance, taking into account the development of problems in their fine motor skills in the future.
Pathogenetic aspects
Today, neurology as a science does not have reliable information about the etiology and pathogenesis of neural amyotrophy. Studies have shown that 70-80% of patients with CMT who underwent genetic testing had duplication of a certain section of chromosome 17. It has been determined that Charcot-Marie-Tooth neural amyotrophy has several forms, probably caused by mutations of various genes. For example, researchers have found that in a form of CMT caused by a mutation in the MFN2 gene encoding the mitochondrial protein, a clot of mitochondria forms, disrupting their movement along the axon.
It has been established that most forms of CMT are associated with damage to the myelin sheath of peripheral nerve fibers; forms with pathology of axons—axial cylinders passing in the center of the nerve fiber—are less common. Degenerative changes also affect the anterior and posterior roots of the spinal cord, neurons of the anterior horns, Gaulle's pathways (spinal pathways of deep sensitivity) and Clark's columns related to the posterior spinocerebellar tract.
Secondarily, as a result of dysfunction of peripheral nerves, muscle atrophy develops, affecting certain groups of myofibrils. Further progression of the disease is characterized by displacement of the sarcolemmal nuclei, hyalinization of the affected myofibrils and interstitial proliferation of connective tissue. Subsequently, increasing hyaline degeneration of myofibrils leads to their disintegration.