Chronic nonspecific lung diseases (CNLD) are one of the most important problems of modern pulmonology, representing etiological and pathomorphological processes in the respiratory system, accompanied by a protracted productive cough due to damage to the bronchi and parenchyma. The group of these chronic diseases includes pathological disorders in the respiratory organs, which appear due to various causes and mechanisms of development, but have similar signs of progression and similar morphofunctional dysfunctions.
What is CNLD
Traditionally, chronic nonspecific lung diseases include the following groups of pulmonary diseases:
- Chronic bronchitis.
- Bronchial asthma.
- Emphysema.
- Bronchiectasis.
- Chronic pneumonia.
- Pneumosclerosis.
However, some authors classify interstitial pathologies of the respiratory system as independent types of NCL. Others object, believing that only chronic bronchitis, emphysema and bronchial asthma are independent manifestations of nonspecific pathologies of the respiratory system. Therefore, the classification of chronic nonspecific lung diseases still raises some questions and even disputes among specialists.
How does Belmondo syndrome manifest?
Pain is one of the most important reactions of the human body to a threat to life, a violation of tissue integrity. Only when we feel pain do we learn that something is wrong with us: we have burned ourselves, damaged ligaments in our legs, worn down our feet to calluses, or splintered our toes.
In addition to unnoticeable pain, patients with this rare disease experience the following difficulties:
- Anhidrosis. A person does not respond to changes in environmental temperature, and, accordingly, body thermoregulation is disrupted;
- Does not notice the urge to go to the toilet;
- There is no fatigue, the body does not realize when it is time to go to bed;
- Due to the threat of muscle numbness, you have to regularly consciously change position;
- Mechanically scratching the skin can cause serious wounds;
- The feeling of hunger is unknown, the patient may become weak and will not even notice it.
Thus, people with Belmondo syndrome have to consciously control all basic physiological needs, since the body is not able to signal a lack of anything.
Reasons for appearance
The main factors causing the manifestation of nonspecific pathologies of the pulmonary system in the population are:
- urban air pollution;
- occupational hazard;
- frequent acute infectious processes;
- bad habits.
COPD is much more often diagnosed in people living in industrial cities, where large amounts (several times higher than the permissible norm) of hazardous substances are found in the air: nitrogen oxide, sulfur and carbon dioxides, dust particles and other components. In such regions, the frequency of diagnosed chronic lung diseases (as a medical and social problem) often reaches the federal level.
Occupational chronic lung pathologies most often occur in people exposed to constant exposure to drafts, gas pollution and dust. In addition, according to numerous studies, smoking people are most susceptible to the risk of nonspecific diseases of the respiratory system.
Other factors leading to chronic nonspecific lung diseases include: frequent and long-lasting acute respiratory viral infections, repeated bronchitis and pneumonia. Prolonged and infectious pathologies of the respiratory system, various types of allergic manifestations and immune disorders can also be the root causes of the development of COPD.
The likelihood of nonspecific disorders in the lungs occurring in a chronic form increases in people over 40 years of age. Moreover, such pathologies are mostly found in men. The list of chronic lung diseases, according to medical statistics, in this case looks like this:
- Chronic bronchitis – about 59%.
- Bronchial asthma – about 36%.
- Bronchiectasis – about 3.5%.
- Other lung diseases – less than 1.5%.
The pathological anatomy of chronic nonspecific lung diseases may be based on one of three scenarios for the development of the disease: bronchitogenic, pneumonogenic and pneumonitogenic causes.
The pathogenesis of bronchitis development is due to the occurrence of disturbances in bronchial patency and the drainage ability of the bronchi. Typically, pathologies related to the classification of obstructive pulmonary diseases develop according to this scheme: chronic bronchitis, asthma, emphysema and bronchiectasis.
Pneumoniogenic and pneumonitogenic mechanisms are associated with the formation of chronic forms of pneumonia and lung abscess, which, in turn, are complications of broncho- or lobar pneumonia.
The outcome of these mechanisms most often are pathologies such as pneumosclerosis (pneumofibrosis, pneumocirrhosis), cardiopulmonary failure and other undesirable consequences. In recent years, COPD has increasingly been considered as the main cause of tuberculosis and lung cancer.
Causes of inflammation
The causes of both acute and chronic inflammation can be different. In particular, they may be as follows:
- Infectious agents such as bacteria, viruses, fungi;
- Injuries such as abrasions, scratches, cuts;
- Damage caused by foreign bodies entering the body;
- Chemical particles: Substances such as silica contained in coal dust cannot be completely broken down or removed from the body and can therefore cause chronic inflammation.
- Autoimmune diseases: that is, diseases in which the body's immune system begins to attack its own tissues or organs. For example, systemic lupus, Rheumatoid arthritis.
What is ulcerative colitis? Causes, symptoms and treatment
CAUTION: Factors such as smoking, obesity, alcohol abuse, stress, old age, low levels of male and female sex hormones, sleep disorders, and a diet containing refined sugar, saturated fats and trans fats contribute to chronic inflammation.
Chronical bronchitis
According to the prevalence, bronchitis can be local or diffuse, according to the type of inflammatory process - catarrhal or mucopurulent. It can be obstructive and non-obstructive, in nature - atrophic, polyposis, deforming.
Clinical manifestations of chronic nonspecific lung disease of this type are expressed in annual, periodically recurring, long-term inflammation in the bronchi. Often, exacerbations of chronic bronchitis occur up to 4 times a year, while the annual duration of this pathology can reach 3-6 months.
A symptomatic sign of chronic bronchitis is a persistent cough accompanied by sputum. During exacerbations, the cough usually becomes more severe, the sputum becomes purulent, sweating and an increase in temperature are added. The outcome of this pathology can be the development of chronic pneumonia, pulmonary atelectasis, emphysema, and pneumofibrosis.
What is inflammation?
Inflammation is a protective method used by the body to get rid of germs, harmful substances, foreign particles, dead cells and tissue. The inflammatory process consists of several successive stages in which cells of the immune system and blood vessels are involved. For chronic inflammation, anti-inflammatory drugs based on cortisone are also used.
Products containing sugar and trans fats, such as margarine, damage tissue and increase inflammation. Foods such as salmon, tomatoes, blueberries, hazelnuts and olive oil have a calming effect on inflammation.
Hyperthyroidism (thyrotoxicosis): causes, symptoms and treatment
Types of inflammation
There are two types of inflammatory processes: acute and chronic.
- Acute inflammation: it occurs suddenly, progresses quickly over several days, reaches its critical (severe) stage and ends.
- Chronic inflammation: It starts slowly and lasts for several months or longer.
Bronchial asthma
There are several types of bronchial asthma: it can be non-atopic, atopic, mixed, aspirin-induced or an occupational disease. This pathology is the second most frequently diagnosed of all nonspecific lung diseases. Their symptoms in adults and children are characterized by hyperreactivity of the bronchial tree, which leads to hypersecretion of bronchial mucus, edema and paroxysmal spasms of the airways.
For any genesis, the clinical manifestations of bronchial asthma are attacks of expiratory dyspnea. The development of such phenomena occurs in three stages:
- Harbingers. They signal the onset of an asthma attack in the form of coughing, mucous discharge from the nose, and the appearance of swelling and redness of the conjunctiva of the eyes.
- Suffocation. It is characterized by the appearance of wheezing, sharp shortness of breath with prolonged exhalation, diffuse cyanosis, and nonproductive cough. During the period of suffocation, the patient needs to lie down so that the head and shoulder girdle are on a hill. In severe cases of suffocation, the patient may die due to respiratory failure.
- Stage of reverse development of the attack. Characterized by sputum separation, decreased wheezing and freer breathing. Gradually, shortness of breath completely disappears.
Between the manifestations of asthma attacks, the condition of patients remains quite satisfactory, provided that clinical recommendations are followed: chronic nonspecific lung disease, with its prolonged course, leads to the development of obstructive emphysema, cor pulmonale, and pulmonary heart failure.
Other names for the disease
The syndrome has nothing to do with the name of the famous French actor . Even the stress is placed on a different syllable: it is correct to say “ bel-mON-da syndrome .” Moreover, the disease is known under this name only in Russia.
Western medicine describes congenital sensory neuropathy with anhidrosis, abbreviated as CIPA (Congenital insensitivity to pain with anhidrosis). The name gives a clear definition and nature of the disease.
The syndrome occurs immediately at birth, is accompanied by disruption of the nervous system and is accompanied by a lack of sweating.
Manifestations of chronic obstructive pulmonary emphysema
The morphological basis of this disease is manifested in a persistent expansion of the lumen of the bronchioles and alveoli due to a chronic obstructive process in the respiratory tract against the background of the development of chronic bronchitis and bronchiolitis. The lung becomes more airy and increases in size.
The clinical picture of this COPD is due to a rapid reduction in the area of gas exchange and a decrease in pulmonary ventilation. Symptoms of this pathological process appear gradually, with the patient experiencing progressive shortness of breath, cough with a small amount of sputum, and weight loss.
Upon examination, barrel-shaped changes in the anatomical structure of the chest, cyanosis of the skin, and changes in the nail plates of the fingers are detected. The pathology, which belongs to the general classification of chronic lung diseases, is often accompanied by infectious complications, pulmonary hemorrhages, and pneumothorax. Respiratory failure can be fatal for the patient.
Diagnostics
Blood is donated strictly on an empty stomach
In many cases, the disease is detected accidentally during cytogenetic analysis. Many patients do not find out about their anomaly until the end of their lives. The diagnosis has no medical significance. The prognosis for people with Jacobs syndrome is good because there is no limitation on life expectancy.
To identify secondary complications of the syndrome, an analysis is used to determine the concentration of sex hormone-binding globulins. The examination is indicated for men with erectile dysfunction and decreased libido. Blood is donated on an empty stomach. Before taking the test, it is recommended to avoid drinking alcoholic beverages, smoking and limiting physical activity. You must inform the laboratory technician or attending physician in advance about taking medications.
Bronchiectasis
The pathological anatomy of chronic nonspecific lung diseases includes changes in the structure of the respiratory tract. Bronchiectasis is characterized by saccular, cylindrical or fusiform dilatations of the bronchi. Such phenomena are called bronchiectasis. They can be local or diffuse, congenital or acquired.
The appearance of congenital chronic nonspecific lung diseases in children is usually caused by disturbances in the development of the structure of the bronchopulmonary system at the stages of the prenatal and postnatal periods. Most often, such pathologies are associated with the development of intrauterine infections, Sievert-Kartagener syndrome, cystic fibrosis, etc.
Signs of the acquired form of bronchiectasis occur against the background of recurrent bronchopneumonia, chronic bronchitis, or the prolonged presence of a foreign body in the bronchi. Bronchiectasis, like many other lung diseases and their symptoms in adults, manifests itself in the form of a cough with sputum production. A distinctive feature in this case is the discharge of yellow-green pus with an odor, and in rare cases, hemoptysis occurs. During exacerbations of this pathology, clinical signs are similar to the course of exacerbations of chronic purulent bronchitis.
Complications of the disease lead to pulmonary hemorrhage, lung abscess, respiratory failure, amyloidosis, purulent meningitis, and sepsis. Any of these conditions is life-threatening for a patient with a history of chronic nonspecific lung disease. In children and adults, by the way, such a pathology is extremely rare: the percentage of congenital bronchiectasis in relation to other nonspecific diseases of the pulmonary system is about two percent.
Course of the disease
The main pathological sign of the disease is a decrease in the number of platelets in the peripheral blood, as a result of which a pronounced hemorrhagic syndrome of the hematopetechial type develops. Thrombocytopenia (decrease in platelet count) leads to a decrease in platelet components of the coagulation system and the development of coagulopathic syndrome (blood clotting disorder).
In idiopathic thrombocytopenia, when the causative factor cannot be identified, hyperproduction of megakaryocytes and platelets is observed in the bone marrow. In immune forms of thrombocytopenia, the destruction of platelets of platelets occurs under the influence of antibodies; in hereditary forms, the shortening of the life of platelets is caused by impaired activity of glycolytic enzymes, a defect in the structure of their membrane, and a decrease in the level of thrombopoietins. Using the radioactive indication method, a sharp shortening of platelet life to 8-24 hours instead of 7-10 days is revealed, in some cases their disappearance.
In children, the appearance of thrombocytopenic purpura is often preceded by acute respiratory viral infections and vaccination (diphtheria, whooping cough, smallpox, measles, polio, influenza). In newborns, thrombocytopenic purpura is congenital, but not genetically determined, since it is associated with transplacental transmission of antiplatelet iso-antibodies (the mother is healthy) and autoantibodies (the mothers suffer from Werlhof's disease) to children. In the genesis of bleeding in thrombocytopenic purpura, in addition to the lamellar factor, the condition of the vascular wall also plays a role.
Chronic pneumonia
Chronic pneumonia, which can combine an inflammatory component, carnification, chronic forms of bronchitis and lung abscesses, bronchiectasis, and pneumofibrosis, poses no less threat to the patient’s life. That is why not all authors agree with the inclusion of this pathology in the classification of lung diseases as an independent nosology. With each exacerbation of pneumonia, a new focus of inflammation appears in the lung tissue and the area of sclerotic changes increases.
Symptoms of chronic pneumonia: constant cough with mucopurulent sputum during remission, purulent sputum during exacerbation, as well as persistent wheezing in the lungs. During the acute period of the disease, there is usually an increase in body temperature, chest pain, and respiratory failure. Often the disease is complicated by pulmonary heart failure, abscesses and gangrene of the lungs.
Is the mutation inherited?
Jacobs syndrome is not inherited. A man with trisomy XYY will not pass on the abnormal number of chromosomes to his sons. The mutation occurs randomly during spermatogenesis. If one of the abnormal sperm penetrates the egg, the baby will have an extra Y chromosome in each of the body's cells.
In some cases, the addition of an extra Y chromosome occurs due to nondisjunction during cell division during early embryonic development. In this case, either a 46, XY karyotype or a 47, XYY karyotype can arise.
Pneumosclerosis
Chronic nonspecific lung diseases with diffuse pneumosclerosis, which occurs with gradual replacement of parenchyma tissue with connective tissue, include a pathology called “pneumosclerosis.” This phenomenon occurs as a result of inflammatory-dystrophic conditions in the lungs and leads to drying out, airlessness and hardening of the lungs. Often this pathology is a consequence of chronic bronchitis, bronchiectasis, COPD, chronic pneumonia, fibrosing alveolitis, tuberculosis and many other inflammatory processes.
The main symptom of pneumosclerosis is shortness of breath, which appears even with little physical effort. Soon it begins to bother you constantly, even at rest. Another sign of this pathology is a cough. Depending on the degree of damage to the lung, pneumosclerosis may manifest itself in the form of a slight cough or a loud thump. Sometimes the clinical picture is complemented by cyanosis of the skin and chest pain. As the connective tissue in the lungs increases, symptoms become more noticeable.
Symptoms
The STD group includes dozens of different diseases. Each of them is caused by specific pathogens and is accompanied by individual symptoms. But there are a number of common symptoms and signs that accompany most sexual diseases. Among them:
- itching and burning in the intimate area;
- altered genital discharge;
- increase in the number of discharges;
- pain in the lower abdomen;
- discomfort or pain during sex;
- rashes in the genital area, etc.
Here we will look at the most common STDs that anyone who is sexually active can become infected with. If any of them are detected, you must urgently contact a specialist: a gynecologist, urologist or venereologist.
Syphilis is one of the most ancient sexually transmitted diseases; its causative agent is the pallidum spirochete. There are three stages of syphilis, and each of them is accompanied by its own symptoms. The infection can remain in the body for a long time (sometimes several years) and not manifest itself in any way externally.
One of the first symptoms of the disease is the appearance of chancre. It occurs in the genital or anal area. Less often - on the fingers. Over time, the rashes spread throughout the body. The patient is worried about aching bones, fever, and headache. In the later stages, vision deteriorates, weakness appears, and immunity decreases. If left untreated, syphilis leads to damage to all organs and systems.
HIV (human immunodeficiency virus) is the most dangerous STD, which in the absence of antiretroviral therapy can develop into AIDS. The incubation period ranges from 1 to 6 months (most often 3 months). Among the first symptoms of the disease are acute tonsillitis, enlargement and inflammation of the cervical lymph nodes, and prolonged low-grade fever.
Chlamydia - the first symptoms appear approximately a week after infection. Infected men and women experience mucous discharge from the genitals, cutting pain when urinating and discomfort during sexual intercourse. Often, infected women experience intermenstrual bleeding and pain in the pelvic area.
Genital herpes is an infectious STD that is caused by the herpes simplex virus type 1 or 2. During primary infection, it may be asymptomatic. After infection, the virus remains in the human body forever and appears externally from time to time. A characteristic symptom of the disease is a rash in the form of small blisters on the genitals and in the anus.
They are accompanied by itching, discomfort and burning when urinating. After a few days, the blisters turn into ulcers and become crusty. There is weakness, increased body temperature and enlarged inguinal lymph nodes. The herpes virus is especially dangerous for pregnant women and requires urgent treatment.
Gonorrhea is a classic sexually transmitted disease that is classified as an STD. Its causative agent, gonococcus, affects the urethra, cervix, pelvic organs, rectum, pharynx and even the eyes. The incubation period is several days. The disease manifests itself with acute symptoms - patients are bothered by purulent discharge from the genitals, pain in the lower abdomen, burning sensation when urinating and discomfort during sex.
Women experience spotting after sexual intercourse. When it affects the rectum, gonorrhea causes localized pain and anal discharge. Complications of gonorrhea include inflammatory diseases of the pelvic organs, testicles and prostate gland, male and female infertility, and termination of pregnancy. In the chronic course of the disease, all organs and systems of the body are affected.
Phthiriasis or pediculosis pubis is a parasitic disease caused by the pubic louse. It is transmitted through sexual contact during contact of partners' hair or due to the common use of bed linen, clothing and personal hygiene items.
The first symptoms appear within a day. The patient is concerned about itching in the hair area, peeling, dermatitis, papules and ulcers occur. If left untreated, lice can spread throughout the body, causing associated diseases.
Trichomoniasis is one of the most common STDs in the world. Caused by Trichomonas. The incubation period ranges from 7 to 28 days. In women, the disease manifests itself more clearly; in men it can be asymptomatic. Patients experience mucous yellowish discharge from the genitals (usually with an unpleasant odor), pain during sexual intercourse, and itching during urination.
When the prostate gland is damaged in men, prostatitis occurs. Trichomoniasis is especially dangerous for pregnant women - it can cause premature birth and other complications.
COLD in pediatrics
Children born prematurely are at increased risk of developing chronic lung diseases in newborns, because the organs of the bronchopulmonary system are formed in the last stages of intrauterine development. Therefore, premature babies are still likely to have partially underdeveloped lungs. Quite common diseases of the bronchopulmonary system in infants are bronchopulmonary dysplasia (BPD) and congenital lung malformations, but other inflammatory pathologies are often diagnosed in them.
Pneumonia is a common condition in young children and is most often a consequence of a cold, sore throat, or can be easily transmitted by airborne droplets. Most children who experience this disease in an acute form in the first 3 years of life develop chronic pneumonia. The protracted and then chronic nature of this pathology is due to a violation of the drainage functions of the bronchi, which provokes the development of hypoventilation, atelectasis, local purulent bronchitis, infection of the bronchopulmonary lymph nodes and destruction of lung tissue.
With all such dysfunctions and diseases of the lungs, their symptoms indicate the presence of deformations and expansions in the structure of the bronchi, as well as signs of chronic bronchitis. This happens due to the early development of chronic pneumonia, while mucus accumulates in the altered small branches of the bronchi.
Predisposing factors for the development of the chronic form of the disease most often are:
- disturbances in the formation and malformations of the bronchopulmonary and vascular systems of the lungs;
- congenital and acquired dysfunctions of the mucociliary apparatus;
- chronic pathologies of ENT organs;
- immunodeficiency disorders;
- unfavorable eco-pathogenic effects of the environment;
- passive smoking;
- unfavorable premorbid background: artificial feeding, diathesis, congenital pathologies of immunogenesis, etc.
Microbiological studies of sputum and bronchial swabs often reveal pneumococcal and staphylococcal infections. In most children, during the period of exacerbation of this chronic nonspecific lung disease, the involvement of viral infections is confirmed. Chronic pneumonia is characterized by the presence of sclerotic changes in the affected areas of the lungs. In this case, cellular lymphoid infiltrates often develop, leading to compression of small airways.
The inflammatory process, which occurs first with prolonged and then chronic pneumonia, gradually subsides, giving way to local pneumosclerosis. In the absence of adequate treatment, as the patient ages, the clinical picture of the disease begins to be dominated by symptoms of bronchiectasis. Often, an adult patient is not even aware of the relationship between the bronchiectasis present in him and an unfavorable acute form of pneumonia suffered in childhood.
Diagnosis of inflammation
Disease history
Concomitant diseases and medications taken should be studied. It is also necessary to find out when the first symptoms appeared, which symptoms predominate, and under what circumstances certain symptoms increase or decrease.
Patient examination
The presence of heat, swelling, swelling, redness in the joint area or other places is checked. Since the joints are the most frequently affected by inflammation, the presence of morning stiffness should be examined in detail, as it may be a symptom of rheumatoid arthritis.
Laboratory research
In cases of acute inflammation, as the body’s “defense mechanism” is activated, the number of white blood cells (leukocytes) in the blood increases. In some diseases with chronic inflammation, anemia may occur. Therefore, a general blood test is mandatory for any inflammatory process.
The presence of inflammation in the body is also indicated by changes in such parameters in the blood as erythrocyte sedimentation rate, the level of C-reactive protein and procalcitonin. To diagnose the underlying disease, as a rule, a biochemical blood test is required to determine the value of electrolytes (sodium, potassium), liver enzymes, etc.
Neuralgia: causes, symptoms and treatment methods for neuralgia
Visualization methods
Since inflammatory processes are observed in most diseases, imaging methods such as ultrasound, CT, and MRI can be used to diagnose diseases. In some cases, a biopsy may also be used to make a definitive diagnosis.
Diagnosis and treatment of childhood COPD
Chronic pneumonia in children can only be diagnosed in a hospital setting with the help of comprehensive clinical and radiological studies using bronchoscopy, bronchography and laboratory tests. X-ray images of the lung in chronic pneumonia show an enhanced pulmonary pattern, which has a clearly defined deformation with a reduction in the volume of individual segments and thickening of the walls of the bronchi.
The stages of exacerbation and remission are determined taking into account the dynamics of the clinical picture, microbiological and cytological examination of sputum and laboratory indicators of inflammatory activity (quantitative ratio of ESR in the blood, shift in the leukocyte formula, positive CRP).
In the treatment of chronic pneumonia in children, the same methods are used as in the treatment of acute pneumonia. The main objectives of the treatment are restoration of the drainage function of the bronchi and normalization of the body’s immunological reactivity. After effective treatment, a sanatorium stage of recovery and regular medical examination in the clinic are recommended. If conservative treatment is ineffective, surgical interventions may be used.
With proper organization of dispensary observation in the clinic and adequate treatment of chronic pneumonia in children, the prognosis of this pathology is relatively favorable. However, there remains a risk of developing other forms of COPD at an older age.
Causes
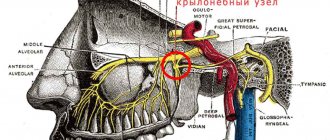
The pathological substrate of Meniere's disease is an increase in the volume of fluid (endolymph) in its cavity and, due to this, an increase in pressure inside the labyrinth. The cause of excess endolymph may be its overproduction, disruption of its circulation or absorption. Under conditions, excess endolymph pressure interferes with the normal conduction of sound waves and impairs trophism in receptor cells. A sharp increase in pressure in the labyrinth provokes an attack of dizziness.
- Viral theory . According to this hypothesis, the onset of the disease is provoked by a viral infection that activates the autoimmune mechanism (cytomegalovirus and herpes simplex virus can be provoking infectious agents).
- Hereditary theory that Ménière's disease is inherited in an autosomal dominant manner . This hypothesis is confirmed by familial cases of Meniere's disease.
- Some authors have been able to obtain data indicating a connection between Meniere's disease and allergies.
- Vegetative theory . According to it, the cause of the development of the disease is a violation of the autonomic innervation of the vessels of the inner ear. Perhaps vascular disorders are a consequence of a malfunction in the secretory activity of labyrinthine cells that produce serotonin and adrenaline.
Among the provoking factors are also
- water-salt metabolism disorders;
- hemodynamic disorders and vascular diseases;
- ear injuries;
- estrogen deficiency.
Classification
According to the predominant syndrome:
- the cochlear form (about 50 percent of all registered cases) begins with hearing disorders;
- vestibular form - 20 percent of cases; in these cases, the disease is a vestibular disorder syndrome;
- classic form - in this case, in the initial stages of the disease, cochlear and vestibular symptoms are combined.
By severity . This classification is based on the duration of attacks and the duration of periods of time when no symptoms are observed.
- for a mild degree , frequent, rapidly passing attacks are typical, alternating with long breaks lasting from several months to several years; with full preservation of performance during the interictal period;
- moderate severity is characterized by the occurrence of frequent attacks lasting up to five hours, after which the patient’s good health is not immediately restored, and the ability to work may be lost for several days;
- severe of one per day to one per week; the patient's ability to work is permanently lost.
I. B. Soldatov’s classification is widely used by clinicians. This classification distinguishes two stages of the disease:
- The reversible stage is characterized by the presence of “light” intervals between attacks; Disturbances in the sound-conducting mechanism are noted, which is what causes hearing loss at this stage. Vestibular symptoms in such patients are transient.
- At the irreversible stage of the disease, the frequency and duration of attacks increase, and the intervals between them shorten and gradually disappear completely. Vestibular syndrome becomes persistent, hearing is persistently and constantly reduced due to not only the sound-conducting mechanism, but also the sound-receiving apparatus of the ear.
Flow
There is an exacerbation phase , during which the symptoms of the disease fully manifest themselves, and a remission stage - a “bright” period characterized by the absence of symptoms. The persistence of some symptoms during remission is a prognostically unfavorable sign.
At the onset of the disease, phases are well defined: exacerbations and remissions have fairly clear boundaries; over time, as the disease progresses, the patient retains some of the symptoms during remission (noise, heaviness in the head, weakness, vestibular syndrome).
Clinical picture
An attack of significant systemic dizziness combined with nausea and repeated vomiting is a specific set of symptoms that manifests Meniere's disease; a similar condition occurs with Meniere's syndrome. Symptoms, as a rule, are so severe that during an attack the patient cannot stand, and sometimes even sit. Symptoms intensify and the condition worsens when trying to change body position.
The attack is accompanied by the following symptoms:
- noise and feeling of fullness in the ear;
- impaired coordination and sense of balance;
- hearing loss;
- paleness of the face;
- severe hyperhidrosis;
- dyspnea;
- tachycardia;
- rotatory nystagmus, more pronounced when the patient lies on the affected side.
The duration of the attack can vary from several minutes to several days; more often - from two to eight hours. After the end of the attack, the patient continues to feel decreased hearing for some time, noise in the ear on the affected side, heaviness in the head, and a slight lack of coordination; a change in gait is objectively noted. Over time, these symptoms become more pronounced and persistent, which is directly related to the progression of the disease.
Factors that can provoke another attack in Meniere's disease:
- overwork;
- stress, nervous shock;
- tobacco smoke;
- hyperthermia;
- drinking alcohol;
- binge eating;
- loud noise;
- medical manipulations in the ear.
One of the main symptoms - hearing loss - increases with each new attack, gradually turning into complete deafness. It is noteworthy that with the onset of complete deafness, attacks of dizziness cease.
Scope of examination, diagnosis
- otoscopy - allows you to exclude inflammatory diseases, since it reveals the absence of pathological changes in the external auditory canal and eardrum;
- audiometry in Meniere's disease reveals a mixed nature of hearing loss; and as it progresses, sensory hearing loss begins to prevail;
- electrocochleography;
- acoustic impedance measurement;
- promontorial test;
- otoacoustic emissions;
- vestibulometry;
- stabilography;
- indirect otolitometry;
- electronystagmography and videooculography are needed to study spontaneous nystagmus; with Meniere's disease, the horizontal rotator type is identified;
- MRI of the brain is performed to exclude acoustic neuroma;
- consultation with a neurologist;
- electroencephalography
- ECHO-encephalography to detect or exclude intracranial hypertension;
- rheoencephalography to study the condition of cerebral vessels;
- Doppler ultrasound of cerebral vessels;
- Diagnosis of increased endolymphatic pressure is carried out using the glycerol test. To perform this diagnostic test, the patient takes a mixture of glycerol, water and fruit juice. The concentration of glycerol is determined at the rate of one and a half grams of glycerol per kilogram of weight. If, after 2-3 hours, threshold audiometry reveals a decrease in hearing thresholds of 10 DB at three or more sound frequencies, or 5 DB for all frequencies, the test is considered positive.
Differential diagnosis is carried out with acute labyrinthitis, inflammation of the eustachian tube, otosclerosis, otitis, oncological lesions of the auditory nerve, labyrinth fistula, vestibular neuronitis, psychogenic disorders.
Treatment
Pharmacotherapy for Meniere's disease, as a rule, leads to a decrease in noise in the ear, a shortening of the duration of attacks and a decrease in their frequency, and a decrease in the severity of attacks; however, it does not prevent progression of hearing loss.
Therapy for this disease should be carried out against the background of a healthy lifestyle, proper daily routine and psychological comfort.
Comprehensive long-term treatment of Meniere's disease involves the use of medications that improve microcirculation in the vessels of the structures of the inner ear and reduce the permeability of capillary walls; diuretics, neuroprotective agents, venotonics, atropine-like drugs.
The attack is relieved by combinations of neuroleptics, atropine and scopolamine, antihistamines, and dehydrating agents.
If complex drug therapy is ineffective, surgical intervention is resorted to.
Diagnosis of chronic nonspecific lung diseases in adults
The identification of various forms of COPD is carried out by a pulmonologist. In this case, the features of the clinical manifestations of the pathology are taken into account, as well as the results of laboratory and instrumental examinations:
- To diagnose the pathological process, it is necessary to conduct a survey radiography, which, if necessary, can be supplemented with linear or computed tomography of the chest. Traditional chest radiography remains the main option for initial examination of the respiratory system in children and adults to this day. This technique has the lowest radiation exposure, is quite informative and accessible. It is based on the indications of a survey radiograph that the need to use additional or special research methods is determined. Using X-rays of the lungs, it is possible to dynamically monitor the development of the pathological process. This allows you to adjust therapy if necessary.
- To identify structural changes in the bronchial tree, bronchoscopy, angiopulmonography and bronchography are performed (if necessary, sputum tests or biopsy may be prescribed).
- The activity of the pathological process and the nature of its occurrence can be determined by examining sputum or microscopic and microbiological swabs from the bronchi.
- The functional reserves of the bronchopulmonary system can be assessed by examining respiratory function (external respiration functions).
- Signs of hypertrophic changes in the right ventricle of the heart can be determined using echocardiography and ECG.
Based on the results of the study of morphological changes in the respiratory system, the doctor will be able to give appropriate clinical recommendations. Chronic nonspecific lung diseases require constant monitoring and treatment.
Etiology, pathogenesis and routes of infection
Once in the body, the prion settles on the surface of the cell, interacting with normal proteins and changing their structure to pathological.
Pathological proteins accumulating on the cell surface block processes occurring on the membrane, which leads to cell death.
Proteins accumulating on the cell surface trigger apoptosis (the programmed process of cell death).
The cell, trying to get rid of proteins on the surface, begins to produce reactive oxygen compounds, but the protein on the surface prevents them from leaving the cell. Active substances destroy the cell itself.
Inflammatory processes begin around the affected cells with the participation of highly active enzymes that affect neighboring healthy cells.
Treatment of COPD in adults
Therapy for nonspecific lung diseases is often determined by etiological factors, pathogenetic mechanisms, the degree of morphofunctional changes and the severity of the process. Nevertheless, it is possible to identify some generally accepted methods for treating independent manifestations of COPD.
In order to relieve infectious and inflammatory pathologies in the bronchopulmonary system, antibacterial agents are selected depending on the sensitivity of the microflora. Bronchodilator, expectorant and secretolytic drugs must be prescribed.
Bronchoalveolar lavage is used to sanitize the bronchi. At this stage, physiotherapy, postural drainage and vibration massage of the chest are usually prescribed. If respiratory failure occurs, the use of bronchodilators and oxygen therapy is recommended.
At the remission stage, it is recommended to undergo clinical observation by a pulmonologist, sanatorium-resort treatment, exercise therapy, use of speleotherapy and aerophytotherapy techniques, as well as taking herbal adaptogens and immunomodulators. In some cases, it is advisable to prescribe glucocorticosteroids. To successfully control the manifestations of chronic nonspecific lung diseases and associated pathologies, it is necessary to select basic therapy.
The question of surgical intervention for COLD is raised only in cases of clinical manifestations of persistent local morphological changes in the patient’s respiratory system. In this case, they usually resort to resection of the affected areas. With the development of bilateral diffuse pneumosclerosis, lung transplantation may be recommended.
Treatment
The main emphasis in the treatment of Werlhof's disease will be aimed at localizing hemorrhagic syndromes, preventing anemia and relapses. The most effective antihemorrhagic agent will be blood or red blood cell transfusions at short intervals of up to 5 days.
The complex also uses vasoconstricting drugs. For local bleeding, lotions with thrombin or hemophobin are recommended. In cases of the disease with pronounced anemia, general therapy will also be supplemented with iron supplements.
One of the most effective methods of treating Werlhof's disease is removal of the spleen (splenectomy). Such surgical intervention is indicated for exacerbations of bleeding, the development of anemia, and in cases where conservative therapy does not have a positive effect.
When treating Werlhof's disease in children, bed rest should be observed during the exacerbation of all symptoms, and subsequently it should be switched to semi-bed rest. During therapy, the child should receive a complete, balanced diet; it should be high in calories and easily digestible. If there is bleeding in the oral mucosa, food must be refrigerated.
It is permissible to use glucocorticoids and, if they have no effect, immunosuppressants. In children, along with adults, the splenectomy method is used if conservative therapy does not produce positive results.
Werlhof's disease during pregnancy dates back to the beginning of the 18th century. led to almost one hundred percent mortality in mothers and fifty percent in children. Now that medicine has stepped far forward, with timely and high-quality care provided to the mother, the outcome is absolutely favorable and this disease cannot be a contraindication to pregnancy and childbirth.
It is important that the woman is under the constant close supervision of doctors who will adjust the drugs used and their dosages in order to avoid side effects on the fetus. Surgical intervention to remove the spleen will be indicated only in cases of struggle for the life of the mother.
Alternative Treatments
Treatment of hyperhydropexic syndrome at home is unacceptable. The use of folk remedies is prohibited. The main task is to restore the water-salt balance, and traditional medicine is not able to cope with this. The only thing you need to do is follow a low-salt diet, monitor the amount of fluid consumed and engage in light sports.
Nutrition
In case of syndrome of inappropriate secretion of antidiuretic hormone, the patient's diet should contain less fat and carbohydrates. The amount of liquid should not exceed 1 liter per day, this includes drinks and other liquid dishes. Not too sweet fruits, fresh vegetables, herbs and lean meats (veal, turkey, chicken and rabbit) are healthy.
Physical exercise
Patients who are overweight need to engage in physical therapy, swimming, and aerobics. Sanitary spa treatment is also useful.
Symptoms characteristic of the disease
Meniere's disease has very varied symptoms because it can be caused by other specific diseases of the human body.
The main symptoms of Meniere's syndrome are:
- periodic attacks of dizziness;
- imbalance;
- nausea, vomiting;
- profuse sweating;
- decrease or increase in pressure;
- paleness of the skin surface;
- ringing, tinnitus;
- motor dysfunction;
- hearing impairment;
- headache;
- temperature drop;
- dyspnea;
- increased heart rate;
- uncontrolled movements of the eyeballs.