Hemianopsia - homonymous, bitemporal, quadrant
Bilateral hemianopsia is a neurological disorder characterized by bilateral blindness in half of the visual fields.
Tractus hemianopsia (from the word “path”) is caused by damage to the optical pathways, and central hemianopsia develops when the cortical areas responsible for visual perception are damaged.
In other words, hemianopsia is the loss of half of visible vision on the left or right, but always in both eyes.
Damage to the optic tract usually results in death of the optic nerves. With the central origin of the disease, the optic nerves do not atrophy and continue to function.
Loss of visual fields by origin is divided into acquired and congenital. The congenital variant occurs when the development of the central nervous system is impaired during the period of intrauterine maturation of the fetus.
It is almost always combined with other defects of the nervous system and rarely occurs as an isolated pathology. The acquired variant develops mainly in people whose average age is from 30 to 50 years.
More common in women.
Causes
Hemianopsia occurs when the optic tract, cortex, or subcortical areas are damaged. It follows that it is necessary to look for the nature of damage to the visual system.
- Pathology of cerebral circulation due to arterial blockage due to atherosclerosis or arterial hypertension. They lead to an acute lack of blood in the vessels, as a result of which parts of the brain die from lack of oxygen and nutrients. The type of visual field pathology is determined by the pool and area of the brain in which the blood flow is disrupted. Vision is often impaired when blood supply to the posterior cerebral artery, which supplies the occipital and parietal cortex, is reduced. With a stroke or aneurysm, intracranial pressure increases and hemorrhage into the brain tissue is provoked, and the visual pathways are damaged.
- Inflammation of the meninges and brain parenchyma. Inflammation of the membranes, if localized primarily in subcortical structures, compresses parts of the brain and causes mechanical compression. This impairs the conduction of nerve impulses.
- Volumetric processes in the cranium: tumor, cyst, purulent accumulation.
- Iatrogenic factor. During surgery on the central nervous system, the neurosurgeon may accidentally damage the visual pathways.
- Congenital defects of the central nervous system, accompanied by severe disruption of parts of the brain or hypertension syndrome: dropsy, microcephaly, encephalocele or dysplasia of telencephalon tissue.
A special case of loss of fields, for example, homonymous hemianopia on the left, is determined by the area of brain damage.
Varieties
There are several types of neurological disease:
Homonymous hemianopsia (eponymous hemianopsia)
Unilateral hemianopsia is incomplete loss of vision. Characterized by loss of margins on the right or left. Homonymous hemianopsia occurs when the structures of the central nervous system are damaged by infection, stroke, or mechanical trauma.
Features of the pathology. The homonymous variant is reversible. Thus, right- or left-sided blindness can be a sign of aura during migraine. Aura is the preceding stage of a unilateral headache. Hemianopsia may be one of the signs of a stroke.
Contralateral hemianopsia occurs when there is unilateral damage to the optic nerve. For example, if the optic nerve on the left is damaged, the right lateral visual fields will fall out and right-sided homonymous hemianopsia (right hemianopsia) will occur. If the right optic nerve is damaged, there will be left-sided homonymous hemianopsia.
With complete damage to the lateral geniculate body, complete unilateral hemianopia occurs.
Bitemporal heteronymous hemianopsia
By breaking down each word, you can understand the term. “Bi” means two, “temporal” means the side of the temples of the head. The pathology is manifested by the disappearance of both fields of vision from the temples. Bitemporal hemianopsia occurs when the optic pathway is damaged in the area where the optic nerves intersect.
Heteronymous hemianopsia occurs when the optic nerves are damaged, most often caused by a tumor. Often these are neoplasms in or above the pituitary gland. Temporal hemianopsia is often a symptom of pituitary adenoma.
Binasal hemianopsia
Bi - this is two, that is, on both sides, nasal - meaning the nasal part. The pathology is characterized by bilateral loss of visual fields in the nasal part of the face. Binasal hemianopsia occurs when the optic tract and brain structures are damaged. Also, binasal hemianopsia occurs when the central nervous system is damaged against the background of hydrocele of the brain.
Upper quadrant hemianopsia
Unlike previous types of visual field loss, this quadrant hemianopsia is characterized by loss of the upper half of vision. Superior hemianopsia develops due to damage to the ventral part of the optic tract.
Inferior quadrant hemianopsia
Characterized by loss of lower vision on both sides. Inferoquadrant homonymous hemianopsia occurs when the posterior region of the optic tract or parietal cortex is damaged. Thus, when the parietal cortex is damaged, complete hemianopia occurs.
Clinical picture
Patients suffering from pathology often face everyday discomfort. A visual defect prevents a person from seeing objects in the lost field of vision.
For patients, ordinary events, such as crossing the road, turn into danger: a person cannot see an approaching car.
People are not recommended to drive any vehicle, as there is a risk of accidents.
Lost fields of vision do not even allow you to see the food on the other half of the plate, and difficulties arise when reading, since the other half of the page of the book is not visible. Reading turns into torture for people: people need to make more eye movements.
The neurological illness is accompanied by elementary visual hallucinations. Photopsia is the perception of non-existent ugly phenomena and objects, for example, a suddenly appearing point, flashes, lightning or lights. Often, elementary visual hallucinations with hemianopsia occur after a recent stroke.
Everyday life and basic household things cause psychological discomfort in patients: their actions from the outside seem ridiculous and sloppy.
Some patients develop depression and other neurotic disorders.
As a result of loss of visual fields and a feeling of incapacity, some patients withdraw from social life, preferring to spend time alone.
For patients with hemianopia, the range of possible specialties is limited. Thus, such patients cannot transport passengers or work in places where external assessment of objects is required, for example, in engineering or construction.
The clinical picture of visual impairment, in addition to photopsia, is supplemented by agnosia. This is a neurological disorder characterized by impaired recognition of objects in the visual channel. Patients often exhibit prosopagnosia—impaired recognition of familiar faces. Some patients experience Anton-Babinsky syndrome: people deny the presence of their pathology.
Congenital hemianopsia is often combined with developmental defects in the subcortical and cortical parts of the brain: the thalamus, brain stem and parietal cortex. Therefore, the clinical picture is supplemented by the following pathologies:
- Paresthesia is a perverted sensation. Thus, patients often suffer from tingling skin and complain of flying spots in front of their eyes.
- Violation of deep sensitivity. Patients have impaired pain and tactile perception.
How is the disease detected?
Diagnosis of visual impairment is carried out using visual field testing. The purpose of the express method is to identify field pathologies. In neurological practice, a special hand hammer is used.
A neurologist sits down opposite a person and asks him to close one eye with his palm. The gaze of the open eye is fixed on the doctor's nose. The physician slowly moves the instrument from behind the patient's head from the periphery to the center from all sides.
The patient must be told immediately when he sees the hammer.
Among instrumental methods, perimetry has the greatest diagnostic value. The procedure is carried out using a perimeter.
As a result of the procedure, the doctor receives information about the boundaries of the visual fields for both eyes. Other visual defects are also detected. Computer campimetry is also used.
It identifies disturbances in color perception in various areas of the retina and helps determine the level of disturbance.
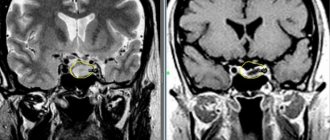
To identify the cause of the disorder, computer and ultrasound diagnostics are used: computer and magnetic resonance imaging, Doppler ultrasound of cerebral vessels. Computer diagnostics helps in choosing treatment tactics, as it allows you to visualize the source of hemorrhage, tumor or abscess.
Treatment
Principles of treatment of hemianopsia:
- Etiological treatment aimed at eliminating the cause. Therapy depends on the identified cause. For example, if computer diagnostics reveals an ischemic focus, medications are prescribed to eliminate hypoxia and cerebral ischemia. If it is cancer, then chemotherapy or surgery is prescribed.
- Socio-psychological recovery. Patients are taught to read and work with text. They are helped to increase the amplitude of eye movement so that an entire line on the page is visible.
If the cause cannot be eliminated, rehabilitation methods are used. The patient is recommended to use glasses with built-in mirrors that compensate for the lack of visibility.
Hemianopsia does not reduce life expectancy, but it can reduce its quality and level. The prognosis for work ability is determined by the etiology and type of anopsia. So, if the disease is detected immediately after a traumatic situation, for example, after a concussion, and immediately responds to treatment, the person fully recovers.
Didn't find a suitable answer? Find a doctor and ask him a question!
Source: https://sortmozg.com/zabolevaniya/gemianopsiya
Diagnostics
Diagnosis of any visual pathology begins with an ophthalmological examination - viziometry, autoreflectometry, examination of the pupil and measurement of intraocular pressure.
To establish hemianopia, you need to perform a topical diagnosis:
- perimetry;
- campimetry.
- Ultrasound Dopplerography;
- MRI;
- computed tomography;
- CT angiography.
Using perimetry, “blind” areas of the visual field are identified. This is the key diagnosis in this case. With homonymous pathology, symmetrical areas are formed: at the temporal part on one side and at the bridge of the nose on the other. That is, the right lobes or the left.
If perimetry cannot be performed due to the patient’s age or other reasons, other diagnostics are used. For example, the doctor holds a stick or towel in his hands and asks the patient to find the middle. With hemianopsia, the patient will divide only part of the stick in half, since he does not see the entire object. Also, the patient does not see the movement of the doctor’s fingers on the affected side of the eye.
With bitemporal pathology, there is a violation of the temporal halves of the visual field for both eyes. With binasal pathology, the central halves (near the nose) fall out.
Using computer campimetry, disturbances in color perception and color perception in a specific area of the visual field are determined.
MRI and CT can determine the etiology of the disease, which will help select the desired treatment algorithm. Using computer diagnostics, it is possible to determine the localization of tumors, areas of brain damage during a stroke, and the extent of traumatic injuries.
CT angiography visualizes the vascular network, using this diagnosis to determine the degree of damage to blood vessels.
Doppler ultrasound is a non-invasive examination method to determine the speed of blood flow.
Homonymous hemianopsia
Homonymous hemianopsia or unilateral - partial blindness with loss of perception of the same right or left halves of the visual field. The disease develops due to a problem in brain function, and not the pathology of the visual organs themselves. Neurological disorders are much more complex.
Homonymous hemianopsia develops due to damage to the optical system or visual pathways. The eyes still function properly, but the information collected is not fully transmitted through the brain and it is unable to process it properly.
The right side of the brain receives information for the left visual field of both eyes, and the left half of the brain receives information for the right.
That is, damage to the left side of the brain leads to the loss of the right half of the visual world of each organ of vision, and damage to the right half leads to the loss of the left side of the visual world of each eye. This is the loss of half the visual field of both eyes on the left or right side.
If vision deteriorates, doctors diagnose relative hemianopsia or hemihypopsia. If, in addition to loss of the visual field, there is a disturbance in the perception of colors while maintaining the perception of white, the diagnosis is hemichromatopsia.
Kinds
There are two types of disease - homonymous and heteronymous, which are divided into several subtypes.
Homonymous hemianopia is divided into:
- quadrant - with this form, the lower or upper field of vision is lost (develops due to damage to the ventral part of the optic tract, the reason lies in partial damage to the fibers of the Graciole bundle);
- contralateral - the patient does not see anything that is in the area of the nose of one eye and the temporal part of the other;
- right-sided and left-sided - depending on the side of the optic tract lesion.
Heteronymous is divided into binasal and bitemporal forms. Binasal - occurs due to compression of the chiasm. It develops during an inflammatory process in the area of the arachnoid membrane and hydrocephalus associated with oncology.
Bitemporal - a violation of the temporal halves of the visual fields, appears when there is a violation of the middle of the interweaving of two optic nerves.
There is a classification according to the place of prevalence and localization - complete, partial, scotoma.
Complications
The type of complication depends on the cause of homonymous hemianopia. The disease itself can lead to complete loss of visual perception if the patient does not take any measures.
Symptoms
Hemianopsia immediately begins with an acute form and accompanies a traumatic brain injury or stroke. Patients complain that entire areas of the visual image disappear from the field of vision or that large spots appear before the eyes - they prevent clear visualization.
Often the acute form of hemianopsia is accompanied by the following symptoms:
- dizziness;
- nausea, vomiting;
- violation of spatial orientation;
- increased blood pressure;
- violation of facial expressions;
- numbness of the limbs;
- speech disorder.
But sometimes the disease occurs without pronounced symptoms: the patient complains of constant headaches, which are accompanied by partial loss of visual fields; unmotivated weakness and general malaise appear. If such symptoms appear, you should immediately see an ophthalmologist or therapist.
Patients with hemianopsia find it difficult to cope with everyday responsibilities and perform normal work. Walking around the city is dangerous: they do not always see approaching vehicles, do not notice many objects on the road surface, and are poorly oriented in space.
When peripheral vision is lost, it is difficult for a person to navigate space, take care of himself, and perform daily work.
A healthy visual system provides a person with central and peripheral vision. With hemianopia, peripheral vision is absent, which leads to disorientation in space. The field of view is the totality of objects that a person sees simultaneously when fixing his gaze on one thing. When part of the visual field is lost, orientation in space is difficult or impossible.
Notes
- Medical Dictionary: Hemianopsia
- Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V (March 2006). “Homonymous hemianopias: clinical-anatomic correlations in 904 cases.” Neurology
.
66
(6): 906–10. DOI:10.1212/01.wnl.0000203913.12088.93. PMID 16567710. Uses deprecated |month= parameter (help) - ↑ 12
eMedicine > Posterior Cerebral Artery Stroke Authors: Christopher Luzzio and Consuelo T Lorenzo. Updated: Jul 15, 2009 - Weinstein, J.M.; Appen, R. E.; Houston, L; Zurhein, G (1987). "Recurrent scintillating scotoma and homonymous hemianopia due to metastatic melanoma." Journal of clinical neuro-ophthalmology 7 (3): 155–60. PMID 2958508.
- Skoromets A. A.
Topical diagnosis of diseases of the nervous system: A guide for doctors.. - 1st ed. - L.: Medicine, 1989. - P. 91-92. — 320 s. — 50,000 copies. — ISBN 5-225-01582-4.
Treatment
Without eliminating the underlying disease that caused the pathology of the visual analyzer, it is impossible to get rid of hemianopsia. Healing from a somatic disease will lead to full or partial restoration of visual fields. Treatment is carried out either by a neurosurgeon or a neurologist.
Treatment of encephalitis, stroke, and traumatic brain injury is carried out in a hospital. Some acute clinical conditions require emergency surgery. The development of a tumor process in the brain requires treatment at an oncology center: the patient is prescribed radiation therapy or chemotherapy.
If a genetic form of pathology is identified, consultation with a geneticist is required. It is impossible to cure a genetic pathology, so patients are prescribed symptomatic treatment. You will have to take medications and treatment for the rest of your life.
Congenital pathology can be eliminated with surgery or drug treatment. The result will depend on the degree of tissue damage, anatomical abnormalities, and concomitant diseases.
What does the ophthalmologist do in this case? He prescribes symptomatic treatment that relieves pain and partially restores visual function. For example, a doctor may prescribe medications that improve blood microcirculation in the tissues of the visual organ. To strengthen the immune system, immunomodulators and vitamin complexes are prescribed. Physiotherapy stimulates the functions of the optic nerve.
Patients are asked to wear special glasses that complement the missing visual picture.
If the underlying condition is not treated, the optic nerve may become damaged. Optic nerve atrophy leads to vision loss and complete blindness. It is important to consult a doctor in a timely manner and undergo medical examination if necessary.
Complications, prognosis and prevention
Today it is impossible to completely avoid the development of hemianopsia. However, it is quite possible to reduce the likelihood of acquiring this disease by following certain rules:
- Avoid contact and intracranial injuries whenever possible;
- promptly identify and treat diseases that may cause the occurrence of this pathology in humans;
- visit an eye doctor, neurologist and other clinicians every year;
- monitor the state of the cardiovascular system.
If the disease does begin to develop, then you need to try to choose a good medical institution that can professionally identify and treat it.
If we talk about the prognosis for the treatment of hemianoptic disease, then its outcome is dictated by such factors as: the severity of development, the characteristics of the treatment, the period of development of visual impairment, the individual characteristics of the body and the age of the sick person, as well as the presence of various complications. Unilateral or bilateral form of the pathology can cause complete or partial loss of vision. The possibility of death cannot be ruled out, especially if the development of the disease is combined with the formation of tumors in the brain area.
Article Rating
Types of disease
Homonymous hemianopsia is usually divided into complete (vision is almost completely absent), partial (part of the picture disappears), quadrant (upper/lower field of vision is impaired) and scotoma. When the occipital lobe of the brain is damaged, contralateral homonymous hemianopia occurs.
In some cases, vision may be impaired due to the formation of a dark spot (scotoma). Scotoma occurs both bilaterally and in the reverse (unilateral) manner. Unilaterally one eye is affected, bilaterally both are affected.
But what could be the causes of yellow whites of the eyes in adults, this information will help you understand.
The video shows a description of the disease:
Bilateral scotoma is usually distinguished into:
- of the same name (with a lesion located above the site of crossing of the optic nerves)
- different names (with a focus located in the area of crossing of the optic nerves). But what a congestive optic disc looks like and how it is treated is indicated here.
With scotoma, pathology may occur, which is usually classified as follows:
- homonymous left-sided hemianopsia (the left side of the eye loses vision);
- homonymous right-sided hemianopsia (the right side of the eye is blinded);
- hemianopsia homonymous superior quadrant (the upper part of the eye is blinded);
- hemianopsia homonymous inferior quadrant (the lower part of the eye is blinded).
Based on the presence of scotomas, a distinction is made between complete (half of vision is lost) and partial.
Homonymous hemianopsia makes it very difficult to see, since with this disease the picture is distorted, which greatly interferes with even reading. A person is not able to fully read the entire text; he sees only one part of what is written.
But what are the causes of flashes in the eyes and what can be done about such a problem is outlined here.
Patients often note that during illness, “nasal” visibility disappears. This may serve as the first alarm bell to contact an ophthalmologist.
Classification
With homonymous hemianopia, loss of equal halves of the visual field occurs: right or left. Taking into account which half falls out, 2 types of pathology are distinguished:
- right-sided;
- left-handed.
Taking into account the location and extent of the pathological process, the following types of symmetrical hemiopia are distinguished:
- Full. The entire half of the visible space is affected, located in the temporal part of one eye and the nasal part of the other eye.
- Partial. Only some of the symmetrical halves of the visual field are darkened.
- Quadrant. The pathological process is localized in the upper (upper quadrant) or lower (inferior quadrant) quarter of the organs of vision.
- Scotoma. It looks like a round or arc-shaped dark spot located in the center of the visible space.
Read in a separate article: Hemangioma of the eye: what is it, treatment in adults and children
Based on the nature of its origin, homonymous hemianopia can also be divided into congenital and acquired.
If the defect is located in the occipital part of the cerebral cortex, then the pathology is contralateral in nature.