For a long time, panic attacks, even at a high medical level, were not considered an independent disease, but were considered only as one of the symptoms of vegetative-vascular dystonia. Only the most modern, more in-depth studies prove that this is rather a psychological (and quite serious) rather than a somatic problem. That is, this means that high blood pressure during panic attacks is not the cause of the attacks, but one of the symptoms accompanying them. However, it has also been proven that frequent changes in pressure can provoke an increase in frequency and worsening of panic attacks.
Symptoms of panic attacks
A panic attack is one of the body's reactions to stress. If a traumatic factor acts for a long time or makes itself felt too often, the anxiety associated with it will certainly affect emotional and physical well-being. A surge in pressure during a panic attack is one of the pathologies that it entails.
Panic attacks, in which blood pressure rises, are a fairly common phenomenon in the modern world. Gender and age play absolutely no role in this. There can be quite a few reasons for the appearance of attacks, but in the vast majority of cases their source is a variety of stressful situations, from which none of us is immune.
Panic attacks are the body’s reaction to fears and stressful situations that arise in a person’s life.
A panic attack can be triggered by:
- inability to tolerate heavy physical activity;
- a number of depressive disorders;
- long-term exposure to traumatic factors;
- the influence of bright flickering light;
- loud, unpleasant sounds;
- frequent drinking of alcohol in large doses;
- smoking, drug addiction.
At the first appearance of an abnormal condition, a person may experience emotional instability, which cannot be controlled and stabilized independently without the help of a specialist.
This may be for no reason:
- irritability;
- nervousness;
- depression;
- apathy to what is happening;
- insomnia or, conversely, increased sleepiness.
Often these conditions are accompanied by severe headaches, dizziness, nausea, lightheadedness, and a feeling of blurred vision.
With constant anxiety, a person’s emotional well-being worsens, he becomes nervous, irritated, depressed
Prevention and recommendations
To prevent the disease from developing into a state of phobia, it is necessary to carry out timely treatment. Experts guarantee a complete cure for the disease. Patients should reconsider their lifestyle, give up bad habits and learn to control their emotions.
Temporary hypertension due to panic attacks is not so much treatable as self-control. In most cases, the developing feeling of fear and anxiety is not justified and is a far-fetched factor. In essence, a person “winds up” negative thoughts to himself, programming himself to be negative.
Drug therapy plus psychotherapeutic sessions will facilitate and improve the quality of life, eliminating the risk of PA and HA.
Panic attacks and high blood pressure: somatic causes of the relationship
Among the diseases that can lead to the occurrence or worsening of panic attacks are:
- diseases of the cardiovascular system (angina pectoris, tachycardia, hypo- and hypertension, VSD - unstable, frequently changing blood pressure, etc.);
- hormonal imbalances (in adolescence, during pregnancy, menstruation);
- diseases of the endocrine system (diabetes mellitus, pancreatitis, hypo- and hyperthyroidism);
- heredity;
- taking certain medications.
All these factors can cause the fact that a certain emotional background (fear, anxiety) begins to be felt at the physical level and manifests itself in the form of rapid heartbeat or, conversely, a sinking heart, numbness of the limbs, a tingling sensation and “goosebumps” on the skin. In addition, a number of biological and hormonal rhythms are disrupted. Despite external manifestations, the reasons for the appearance of symptoms are hidden deep inside.
Increased blood pressure during panic attacks is a common phenomenon in people who suffer from vegetative-vascular dystonia, in which blood pressure is increased
How dangerous is tingling in the heart and why does it occur?
Every person experiences tingling or stabbing pain in the heart at least once in their life; most often they are not associated with serious illnesses.
When to see a doctor?
If your heart tingles, and at the same time the following sensations:
- if tingling is always associated with physical activity and is often repeated;
- give to the left hand or shoulder girdle, jaw, hypochondrium, back;
- accompanied by pallor, fear of death, sweating, fainting, palpitations and interruptions in heart function, edema;
- associated with fever and malaise;
- at rest and at night.
What causes tingling?
The main reasons for tingling in the heart are commonplace:
- intense physical activity. Pain can indicate physiological ischemia (in untrained people) and pathological (myocardial ischemia due to blockage or spasm of the coronary arteries). These sensations are associated with a lack of oxygen, when the vessels cannot cope with the increasing load during exercise;
- infections. When intoxicated by waste products of infectious agents, the heart may feel stabbing. If these sensations do not go away after recovery or get worse, you should consult a doctor. Perhaps this complication is myocarditis;
- cardialgia with depression, neuroses, panic attacks (cardioneurosis). Tingling is possible at rest, against the background of emotional experiences;
- allergy;
- heartburn;
- reaction to drugs: glucocorticoids, cardiac and others;
- stress. Due to excess adrenaline, norepinephrine, and cortisol, the coronary arteries spasm and the heart hurts;
- referred pain in neuralgia, pleurisy, pneumonia, gastritis, cholecystitis, osteochondrosis, tracheitis, pancreatitis, ulcers. Associated with the general innervation of internal organs (vagus nerve, solar plexus, intercostal nerves) and irradiation of pain.
Direct cardiac pain in the form of tingling can be ischemic and non-ischemic (cardialgia). The first include:
- angina pectoris – pain for 5–30 minutes, after emotional or physical stress, is relieved with nitroglycerin, and at rest can radiate to the left arm or shoulder girdle, jaw;
- myocardial infarction - pain similar to angina pectoris, but for more than 30 minutes, not relieved by nitroglycerin, accompanied by fear of death, pallor, shortness of breath, sweating (vegetative manifestations).
True cardialgia or non-ischemic tingling in the heart develops due to:
- myocarditis – infectious or aseptic inflammation of the heart muscle;
- pericarditis;
- heart defects;
- cardiomyopathy (non-inflammatory damage to the myocardium due to hyperthyroidism, viral diseases, congestive heart failure, long-term uncompensated arterial hypertension).
What to do?
If the tingling in the heart area quickly passes and does not recur, then it will be enough to calm down and go out into the fresh air. Take an infusion of valerian, motherwort, a few drops of Corvalol or Valocordin, drink tea with chamomile or mint. In the future, you need to avoid stress, do cardio training, running, swimming.
If the causes of tingling are serious and related to the myocardium, and do not go away for more than 15 minutes, it is important to place an aspirin tablet under the tongue and call an ambulance. Aspirin prevents thrombosis and myocardial infarction. Subsequently, based on the diagnosis, cardiac medications are prescribed (hypotensives, diuretics, coronary vasodilators, aspirin, cholesterol-lowering drugs, nitrates), antibiotics, and glucocorticoids.
For non-cardiac causes, it is important to eliminate the factors that provoke pain. In the case of cardioneurosis (panic attacks, depression, neuroses), the help of a psychologist is necessary, possibly taking antidepressants and anti-anxiety medications. A short course of phenazepam – up to seven days – is effective.
Additional examinations
Designed to exclude cardiac and non-cardiac diseases that provoke tingling:
- ECG: normal, with exercise (cycle track, treadmill test), 24-hour Holter monitor, transesophageal electrical stimulation;
- Echocardiography or ultrasound of the heart;
- general clinical and biochemical blood analysis;
- consultation with an endocrinologist, gastroenterologist, neurologist;
- X-ray of the spine and chest;
- Ultrasound of the abdominal cavity and thyroid gland;
- FGDS;
- thyroid hormone levels.
How to reduce blood pressure during a panic attack
If a panic attack occurs and your blood pressure rises as a result, you need to try to calm down and take a few fairly simple but effective measures:
- open the window, thus letting fresh air into the room where you are;
- free yourself from any items of clothing that constrain or squeeze you;
- do an eye massage (press lightly on closed eyelids in a circular motion);
- take Corvalol or valerian, lie quietly for half an hour.
If you witness a panic attack in another person, try to calm down yourself, and also explain to the patient that everything is fine, reassure him. Relaxation and distraction from the obsessive state is an effective way to eliminate the problem without medication.
Signs of a crisis
During a vegetative-vascular crisis, symptoms of panic disorders dominate. The most common symptoms of a crisis during VSD:
- lack of air;
- tachycardia;
- a feeling of pulsation throughout the body and a coma in the throat;
- fever or chills;
- weakness in the limbs;
- tinnitus, blurred vision;
- tremor;
- discomfort in the chest area;
- sensory disturbance;
- crawling sensation;
- fainting state;
- frequent (or involuntary) urination;
- nausea;
- diarrhea;
- gait disturbance (staggering, shuffling);
- aggression, anxiety.
Sometimes people are haunted by the fear of going crazy and nervous tension. During a crisis, symptoms increase rapidly, reaching their peak after 10 minutes.
Important! The deterioration of the condition is not associated with taking medications or somatic diseases. Crises occur as a reaction to post-traumatic stress disorder.
Drug treatment of panic attacks with high blood pressure
Repeated repetition of attacks should be a signal that it is time to contact a specialist for help. Solving these problems is the responsibility of psychotherapists. The more clearly the original source of the traumatic factor is determined, the more effectively it will be possible to cope with attacks and minimize their occurrence in the future. The specialist may also prescribe medications aimed at improving the patient’s psycho-emotional state - antidepressants and tranquilizers. The former are taken regularly in long courses (from six months to a year, extension or cancellation of the course is controlled by the attending physician), the latter - during the feeling of an impending attack, after an attack.
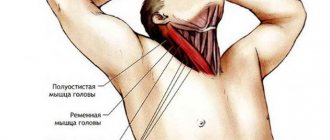
Cervical osteochondrosis as a cause of neurological syndrome
Degenerative processes in the spine, along with neurological signs, also manifest as pain in the heart. Such symptoms in osteochondrosis present difficulties in diagnosing VSD and cardiac pathologies.
With cervical osteochondrosis, the symptoms of VSD are manifested by three syndromes: pain, vascular and trophic. The patient experiences pain in the limbs. The intensity of the symptom depends on the type:
- radiculoalgic – intense paroxysmal pain in the arms;
- neuralgic – aching, prolonged, aggravated by movements;
- myalgic – pain in the muscles when pressed.
Vascular symptoms in adults from osteochondrosis with VSD are manifested by dizziness, pulsating, tingling, burning pain that occurs during movements, changes in skin color (from a marbled pattern to redness). Patients complain of impaired sensitivity in the limbs, tingling in the fingers. When trophism is disrupted, patients' skin becomes thinner, peeling and itching appear.
The clinical picture of VSD intensifies during periods of stress on the nervous system or after physical fatigue. Patients may experience symptoms: attacks of pain in the arms, shoulders, heart area, and head. After taking sedatives and massage, the intensity of symptoms decreases.