Ankylosing spondylitis is called ankylosing spondylitis in international medical terminology. The origin of the disease is in inflammatory changes in the structures of the intervertebral joints. Inflammation promotes their fusion, which is called ankylosis. Due to this process, joint movements are gradually but steadily limited. They become less mobile, move with less amplitude, the process is progressive. As a result, the spine is practically immobilized, and completely. First, mobility decreases, accompanied by pain in the belt area. Then it goes up, rising along the spinal column to the cervical area. In the end, the human body arches “like a question mark” or straightens unnaturally, losing its bends. Diagnosing the disease, especially in the initial stage, is not easy, since medicine has not yet studied exactly the causes that cause it.
Ankylosing spondylitis - diagnosis
Causes of ankylosing spondylitis
The causes of ankylosing spondylitis (ankylosing spondylitis) have not yet been precisely established by science. However, scientists have established a relationship between this disease and the presence of the HLA B27 antigen in humans. This does not mean that the presence of this antigen sooner or later leads to the development of the disease, but indicates a genetic predisposition. There is a theory according to which the HLA B27 antigen makes the joint tissues of people who carry the gene similar to certain types of infections. When a carrier of the gene contracts an infection, the body's immune system produces antibodies to fight it. Antibodies destroy the infection introduced from the outside, after which they “attack” the joints, mistaking them for an infection. However, this is one of the hypotheses.
What is known for certain is that the HLA B27 antigen is present in everyone with ankylosing spondylitis. But not all carriers of this gene necessarily develop ankylosing spondylitis. There is a certain mechanism that triggers the disease program. It could be an infectious disease, even a common cold suffered on the legs. An accidental injury or constant stress can lead to the development of ankylosing spondylitis.
Oddly enough, almost no one in the world is studying ankylosing spondylitis and the causes of its occurrence. The few studies rarely provide new knowledge about this disease. From recent studies, we can only recall experiments conducted on mice, which showed that a disease similar to ankylosing spondylitis in these rodents occurs when three factors are combined: the presence of the HLA B27 antigen, infection from the outside and the presence of T-lymphocytes in the blood. If the mouse was kept in sterile conditions, or the thymus, the organ responsible for the production of T-lymphocytes, was removed, the disease did not develop.
Due to the fact that the mechanism of development of ankylosing spondylitis has not been studied, it is difficult to talk about any prevention. Obviously, people who are carriers of the HLA B27 antigen should monitor their health more closely, avoid traumatic situations, and treat infectious diseases in a timely manner. People who already have ankylosing spondylitis can only prevent complications and slow down the development of spondyloarthritis through constant therapy, physical therapy, and sanatorium treatment.
Basic pathological reflexes
Reflex is the body’s reaction to external stimuli. When there is a disturbance in the functioning of the brain or nervous system, pathological reflexes arise, which are manifested by pathology of motor reactions. In neurological practice, they serve as beacons for identifying various diseases.
Classification of pathological reflexes
Pathological reflexes are divided into the following groups:
- Reflexes of the upper limbs. This group includes pathological carpal reflexes, an unhealthy response to external stimuli of the upper extremities. May manifest as involuntary grasping and holding of an object. They occur when the skin of the palms at the base of the fingers is irritated.
- Reflexes of the lower extremities. These include pathological foot reflexes, reactions to tapping with a hammer in the form of flexion or extension of the phalanges of the toes, and flexion of the foot.
- Reflexes of the oral muscles are pathological contractions of the facial muscles.
Is treatment possible?
Pathological reflexes in neurology themselves are not treated, since this is not a separate disease, but only a symptom of some mental disorder. They indicate problems with the functioning of the brain and nervous system.
Therefore, it is necessary, first of all, to look for the reason for their appearance. Only after a doctor has made a diagnosis can we talk about specific treatment, because it is necessary to treat the cause itself, and not its manifestations.
Pathological reflexes can only help in determining the disease and its severity.
Source: //FB.ru/article/253494/osnovnyie-patologicheskie-refleksyi
Joint pain is a symptom of ankylosing spondylitis
Ankylosing spondylitis (ankylosing spondylitis) does not develop asymptomatically, but the first manifestations of this disease are often missed not only by doctors, but also by patients. The first and most common symptoms are pain in the sacral area, which is often mistaken for sciatica, a constant feeling of fatigue and joint pain. More specific is the so-called “morning” syndrome, when, upon waking up after a night’s sleep, a person cannot move his limbs for some time. Stiffness in the joints usually goes away after half an hour.
Joint pain is characteristic of many diseases, but ankylosing spondylitis is distinguished by the fact that in this case the pain is not eliminated by resting the joint. On the contrary, exercise can bring relief.
Ankylosing spondylitis can occur in three forms: central, rhizomelic and peripheral. In the first two forms, the symptoms are pain in the spine, developing stoop, and the inability to straighten up on your own. In the peripheral form, the disease begins with damage to the knee and ankle joints. Swollen knee joints are one of the reasons to suspect the disease.
Night pain is another symptom of Beheterew's disease. They usually get worse towards the morning. During the day, after noon, they can almost completely disappear.
Ankylosing spondylitis may be indicated by symptoms not only from the joints, but also from other organs and systems of the body. A frequent accompanying symptom is inflammation in the organs of vision. Patients with ankylosing spondylitis experience problems with the respiratory system due to abnormal shape of the chest.
As the disease progresses, the patient's posture changes due to the disappearance of the physiological curves of the spine. The lower back becomes unnaturally straight, a person loses the ability to bend not only back and forth, but also to the sides (this sign helps doctors distinguish patients with ankylosing spondylitis from patients with a severe form of osteochondrosis). Next, the root joints—the hip and shoulder—are affected. Usually the disease “goes” from the bottom up, so the cervical vertebrae are the last to be affected and lose mobility.
Inflammatory processes in the joints are often accompanied by a slight increase in temperature and increased ESR in the blood.
Symptoms of the disease
Cardiovascular symptoms are noted: aortitis, pericarditis, aortic valve insufficiency, heart rhythm disturbances. Kidney amyloidosis is possible.
Thus, the symptoms of ankylosing spondylitis in women and men may be as follows
- feeling of stiffness in the morning;
- pain and stiffness in the spine, sensations intensify at rest;
- asymmetric oligoarthritis, affecting the hip, shoulder, large joints of the lower extremities, as well as small joints of the feet and hands;
- bilateral sacroiliitis;
- enthesopathies - an inflammatory process of ligaments, tendons and places where they are attached to bones;
- intermittent pain in the buttocks.
Extra-articular lesions can affect a number of systems:
- respiratory;
- digestive;
- cardiovascular;
- visual (mucous membranes of the eyes).
If you read this or that commentary with descriptions of the course of the disease, you can get confirmation that in all patients the disease progresses differently, as evidenced by each thematic forum of patients. Symptoms appear less frequently in women than in men.
Diagnosis of ankylosing spondylitis
Diagnostic signs of ankylosing spondylitis: According to the recommendation of the Institute of Rheumatology of the Russian Academy of Medical Sciences, 1997
1. Pain in the lumbar region that does not go away with rest, is relieved by movement and lasts more than 3 months; 2. Limitation of mobility in the lumbar spine in the sagittal and frontal planes; 3. Limitation of respiratory excursion of the chest relative to normal values according to age and gender; 4. Bilateral sacroiliitis stage II-IV.
The diagnosis is considered reliable if the patient has the fourth sign in combination with any other of the first three.
The diagnosis of ankylosing spondylitis (ankylosing spondylitis) is often made only when the disease has already progressed to advanced or severe forms. This is partly due to the lack of knowledge of the disease, partly to the commonality of its first symptoms. Doctors often confuse ankylosing spondylitis with other joint diseases; early signs are often attributed to osteochondrosis.
If ankylosing spondylitis is suspected, an x-ray examination is required. This diagnostic method still remains the most common and is considered the most reliable. The patient takes a photo of the pelvic area. Changes in the sacroiliac joints are a reason for the doctor to suspect ankylosing spondylitis. At the first stage of the disease, the image will show a widening of the joint space and blurred contours of the joints. At the second stage, isolated erosions of the articular tissue will be visible on the image. On the third - partial ankylosis (fixation) of the sacroiliac joints. The fourth stage is pronounced complete ankylosis.
However, changes in the joints in the early stages of ankylosing spondylitis are not always visible on radiographs. A more sensitive method in this regard is magnetic resonance imaging. Unfortunately, there are few such devices in Russian cities, and such studies are carried out extremely rarely.
If ankylosing spondylitis is suspected, a test is carried out to determine the presence of the HLA B27 antigen in a person, since its presence indicates a hereditary predisposition to ankylosing spondylitis. This antigen is usually detected in 80-90 percent of patients.
An additional sign of the presence of the disease can be an increased ESR. But this diagnostic method can only be used in combination with others, since a high ESR only indicates that an inflammatory process is occurring in the body. This process does not necessarily occur in the joints, as in ankylosing spondylitis. Ankylosing spondylitis is characterized by an ESR of 30-60 mm/h.
The doctor makes a diagnosis of ankylosing spondylitis based on X-ray data and clinical manifestations - constant lower back pain lasting at least three months, the presence of morning immobility syndrome, which disappears after exercise, limited mobility in the lower parts of the spine, age-inappropriate restrictions on respiratory excursion.
What else is characterized by pathology?
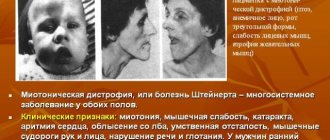
What symptoms characterize the cerebral Rossolimo-Melkersson-Rosenthal syndrome? Initially, it is necessary to mention that Rossolimo is the name of the third doctor who in 1901 described macrocheilitis (a disease of the lips, an increase in their size) combined with facial nerve paresis. Melkersson did this later. But since Rossolimo’s description of the disease, his last name is sometimes used in the name of the pathology.
The cerebral syndrome is detected during an objective examination. It can be expressed as:
- headaches (migraines);
- facial asymmetry;
- paralysis of facial facial muscles;
- Bell's symptom, lagophthalmos;
- xerophthalmia;
- hyperacusis;
- dysarthria;
- angioedema of the face (usually lips);
- tongue folds and macroglossia;
- dysgeusia and ageusia;
- granulomatous cheilitis.
The cerebral syndrome is detected during an objective examination. It can be expressed as:
- headaches (migraines);
- facial asymmetry;
- paralysis of facial facial muscles;
- Bell's symptom, lagophthalmos;
- xerophthalmia;
- hyperacusis;
- dysarthria;
- angioedema of the face (usually lips);
- tongue folds and macroglossia;
- dysgeusia and ageusia;
- granulomatous cheilitis.
Treatment of ankylosing spondylitis, types of treatment
Treatment of ankylosing spondylitis: therapeutic exercises, sports, physiotherapy to avoid incorrect positions or stiffness of the spine and joints. Correct posture should be maintained - this will not allow the spine to lock into an undesirable position. You should sit upright, with maximum extension in the lumbar spine. Sleep on a flat surface and not too soft a bed, and in the early stages - without a pillow and a cushion under the head, so as not to increase cervical lordosis, or on the stomach without a pillow. In more advanced stages, if you sleep on your back, use a thin pillow or place a bolster under your neck, trying to keep your legs straight while sleeping. In the advanced stage of the disease, running, contact sports, and static loads on the spine are contraindicated, but swimming is beneficial.
New targeted medications neutralize negatively acting mediators, thus stopping the inflammatory chain reaction. These drugs are perceived by the patient’s body as natural protein substances, and based on them they belong to a group of drugs called “biological agents”. The emergence of these drugs is the result of intensive biotechnological research, that is, they have nothing to do with homeopathy or alternative treatments. Their second name is “TNF-a blockers,” and one of them is infliximab or Remicade.
Infliximab (Remicade) has proven itself in the treatment of patients suffering from ankylosing spondylitis. Therefore, since 1999/2000, this drug has been approved for use as a therapeutic agent. This drug blocks precisely those pathological mechanisms that cause the inflammatory process and contribute to its further development, without affecting other important protective processes in the body. Therefore, an effect is achieved that could not or rarely was achieved with the help of available medications: effectively preventing the further development of inflammation and thereby maintaining the mobility of the spine and joints.
Effective suppression of inflammation with the drug infliximab (Remicade) may purportedly prevent the dreaded ankylosis of the spine that occurs in ankylosing spondylitis, experts say.
In most cases, it is necessary to use non-steroidal anti-inflammatory drugs: delagil, plaquenil or sulfosalazine (the dosage is selected by the doctor).
In addition to drug therapy for ankylosing spondylitis, the patient should be provided with: sufficient sleep in the correct position, emotional comfort, optimal motor activity, absence of foci of chronic infection, constant physical exercise, and annual spa treatment. Dosed hardening procedures are useful. Manual therapy and therapeutic massage can be used with extreme caution (it is better not to massage the tendon attachment points).
It is worth refraining from physical procedures during an exacerbation.
It should be understood: ankylosing spondylitis will remain with patients forever. But the quality of life and the phase of the disease (remission or exacerbation) depend on proper treatment.
Physiotherapy for ankylosing spondylitis
Physiotherapeutic procedures for patients with ankylosing spondylitis are usually used in conjunction with drug therapy, during spa treatment and to prolong periods of remission. The most common physiotherapeutic procedures are magnetic therapy, heat therapy and cryotherapy. Doctors disagree about the effectiveness of each of these drugs, as do patients themselves.
Magnetic therapy causes the least complaints. Treatment with a magnetic field almost always brings at least short-term relief to patients with ankylosing spondylitis. Due to the fact that many patients find it difficult to travel to the clinic for procedures, they often purchase devices for conducting magnetic therapy at home.
Treatment of ankylosing spondylitis with heat is also easy to carry out at home, however, practice shows that in some cases heating pads or paraffin applications on sore joints can cause even greater inflammation. A bath has a positive effect, but a hot bath can increase swelling of the joints.
Most of the controversy is around cryotherapy, that is, the treatment of ankylosing spondylitis with cold. Most likely, this is due to a sharp deterioration in the patient’s general condition, which is almost always noted after a cryotherapy session. Many doctors immediately warn patients that after the first session all joints may become inflamed. But this does not mean that cryotherapy only brings harm. A number of patients experienced significant improvement after a week of treatment.
During sanatorium-resort treatment, patients with ankylosing spondylitis are prescribed sodium chloride baths, which have an anti-inflammatory and analgesic effect, as well as bischofite baths.
Massage and manual therapy are also used to treat ankylosing spondylitis when the disease is in remission. Almost all doctors are inclined to believe that massage should not be intense, as this can only provoke an inflammatory process. Traditional medicine argues with this opinion. There are cases where the condition of patients with ankylosing spondylitis improved significantly after courses of hard massage conducted by traditional healers who are not recognized by official medicine.
From all of the above, it follows that there is no clear opinion on any physiotherapeutic method of treating ankylosing spondylitis, and the patient has to rely on his own intuition and the reactions of his own body when choosing.
Literature
- Gusev E.I., Konovalov A.N. Burd G.S. Neurology and neurosurgery. - M.: Medicine, 2000. - 656 p. — ISBN 5-225-00969-7.
- G. I. Rossolimo: Pathological spinal reflexes. Journal of Neuropathology and Psychiatry, Moscow. 1902, 2:239.
- GIRossolimo: Der Zehenreflex (ein speziell pathologischer Sehnenreflex. Neurologisches Centralblatt, Leipzig, 1908, 27: 452.
Rossolimo's symptom refers to pathological extensor signs. There are carpal and foot pathological reflex Rossolimo. The presence of this sign indicates damage to the pyramidal tracts of the spinal cord and trunk.
The technique for inducing the upper, wrist reflex is simple: the examining doctor makes a jerky tap with his hand on the patient’s fingertips. With a positive symptom, the fingers bend, and the patient’s hand seems to be trying to “grab” the hand of the examining doctor.
Rossolimo's foot sign is caused by the hammer. A jerky blow of the hammer on the distal phalanges of the toes leads to their flexion. This flexion is sometimes called “toe nodding.” In this case, fingers 2-5 are usually bent, while the first finger remains in one place. The upper and lower reflexes are checked alternately on each side. The severity and localization of the positive pathological reflex allows us to establish a more accurate pathological diagnosis.
The reflex was described by the Russian neurologist Grigory Ivanovich Rossolimo at the beginning of the 20th century and is one of the important components of a standard neurological examination. A positive symptom occurs in the following conditions: multiple sclerosis, diffuse and local brain damage, myelopathy and many other diseases.
Author of the article: Alexey Borisov (neurologist) Practicing neurologist. Graduated from Irkutsk State Medical University. Works in the faculty clinic of nervous diseases.
Corticosteroids in the treatment of ankylosing spondylitis
Corticosteroid hormones are produced by the human adrenal glands as the body's response to any inflammatory process. Quite a long time ago, in 1949, scientists found a way to artificially synthesize these hormones and administer them in high doses to the patient to relieve the inflammatory process.
This therapy has found widespread use for the treatment of patients with ankylosing spondylitis. However, it soon turned out that corticosteroids, while relieving inflammation in the joints, have a number of negative effects on the body. Like any hormonal drugs, artificially obtained corticosteroid hormones are addictive, physical and mental. With regular use of corticosteroids, the human body stops producing this hormone itself, and the adrenal glands atrophy. Excess weight, the appearance of facial hair, stomach ulcers - these are not all the negative consequences of long-term use of corticosteroids. Osteoporosis caused by taking corticosteroids is very dangerous for patients with ankylosing spondylitis. Increased fragility of bones leads to fractures, and forced immobility due to plaster can be fatal for patients with ankylosing spondylitis.
However, despite all the risks, treatment with corticosteroid hormones can provide a significant therapeutic effect and improve the patient's condition. Therefore, the question of whether the use of corticosteroids is justified in each case must be decided individually. It is necessary to prevent in time or at least minimize the harmful effects of the drugs used. Thus, drugs in the form of tablets, for example, prednisolone, are taken at the same time, with plenty of liquids that coat the stomach - jelly or kefir, to reduce the harmful effects on the stomach. If hormones are administered by injection, the patient should focus on preventing osteoporosis, that is, devote more time to physical therapy. During movement, more calcium enters the bones, strengthening them.
If inflammation is concentrated in one joint, local infusions of drugs containing corticosteroids are often used. For example, depomedrol or Kenalog. These injections are usually one-time and provide temporary but significant relief. In addition, a single administration of the drug does not cause side effects.
Consequences of Melkersson-Rosenthal syndrome
The syndrome quickly becomes chronic. This greatly affects a person’s appearance, which is distorted and disfigured by swelling. Against this background, depression and mental disorders often occur. Due to enlarged lips and their inactivity, a person has difficulty chewing and swallowing, and speech distortion is observed.
In the cracks that appear during swelling, harmful bacteria can appear that cause infectious diseases. This also applies to language. Sometimes it becomes covered with cracks. In addition, the risk of this increases due to injury to the swollen mucous membrane by the teeth, for example, while chewing food.
People suffering from this disease are recommended to eat more liquid foods: first courses, various cereals and dairy products. This food is easier to chew and reduces the likelihood of injury to the oral mucosa. Fruits and vegetables are also healthy, but they need to be cut into small pieces or added to salads. It is better to chop large pieces of any food while eating with cutlery.
The syndrome quickly becomes chronic. This greatly affects a person’s appearance, which is distorted and disfigured by swelling. Against this background, depression and mental disorders often occur. Due to enlarged lips and their inactivity, a person has difficulty chewing and swallowing, and speech distortion is observed.
In the cracks that appear during swelling, harmful bacteria can appear that cause infectious diseases. This also applies to language. Sometimes it becomes covered with cracks. In addition, the risk of this increases due to injury to the swollen mucous membrane by the teeth, for example, while chewing food.
{amp}gt;Incidence rate (per 100,000 people)
Prognosis for ankylosing spondylitis
Modern medicine offers ways, if not to cure, then at least to delay the development of ankylosing spondylitis with the help of various medications. Many of them have serious side effects, and some patients prefer to resort to traditional medicine: herbs, massages, baths.
The course of ankylosing spondylitis is accompanied by a change in inflammatory phases and phases of remission. During remission, the patient experiences significant relief, but official statistics do not know cases of complete recovery.
Treatment of ankylosing spondylitis with stem cells
Ankylosing spondylitis is a disease associated with inflammation of the joints of the axial skeleton (intervertebral, costovertebral, sacroiliac) and involvement of internal organs (heart, aorta, kidneys) in the process.
Bechterew's disease tends to have a chronic progressive course. Nikolai Ostrovsky had a classic case of advanced spinal inflammation: immobility and blindness. On average, about 3 people out of a thousand suffer from ankylosing spondylitis in Russia.
Ankylosing spondylitis develops as a result of latent infections in people who have a hereditary predisposition and certain genetic characteristics. In ankylosing spondylitis, inflammation initially affects the junction of the sacrum and ilium; then spreads to the lumbar spine and “creeps” up the entire spine. In the future, the inflammatory process can affect any joints of the body - from the hip to the finger joints.
In many cases, joint inflammation in ankylosing spondylitis can be easily suppressed with the help of medications. It is much worse that with ankylosing spondylitis, “ossification” of the spinal ligaments, its intervertebral joints and discs occurs. There is a gradual process of “fusion” of the vertebrae with each other, the spine loses its flexibility and mobility.
Symptoms of ankylosing spondylitis may initially be very similar to the symptoms of osteochondrosis. The patient complains of pain in the lumbar region. Later, lumbar pain is accompanied by swelling and tenderness of one or more joints, pronounced morning stiffness of the lower back, which disappears by lunchtime.
Ankylosing spondylitis most often begins at a young age of the patient, at 20 - 30 years old. In half of the patients, already at the very beginning of the disease, inflammation of the eyes (redness and a feeling of “sand in the eyes”), increased body temperature and weight loss can be detected.
But the main symptom of ankylosing spondylitis is increasing stiffness of the spine and limited mobility of the chest during breathing movements. A sick person moves as if he had a stick inserted instead of a spine - the patient has to bend and turn with his whole body.
Ankylosing spondylitis is dangerous not only because over time it immobilizes the entire spine and joints, but also due to its complications. Of these complications, the greatest danger is damage to the heart and aorta, which occurs in 20% of patients and is manifested by shortness of breath, chest pain and interruptions in heart function. A third of patients develop amyloidosis, a degeneration of the kidneys that leads to chronic renal failure. Reduced chest mobility contributes to lung diseases.
The first and most important rule is that treatment of ankylosing spondylitis with stem cells should begin when its first symptoms appear, before “ossification” of the entire spine and inflamed joints has occurred.
The effect of the introduced stem cells for the treatment of ankylosing spondylitis is aimed at stopping the “ossification” of the spinal ligaments, its intervertebral joints and discs. And also to prevent the process of “fusion” of the vertebrae with each other, restoring its flexibility and mobility.
After treatment of ankylosing spondylitis with stem cells, the range of motion in the joints and spine significantly increases, pain decreases, and timely treatment with stem cells will avoid damage to the heart and aorta, kidneys and lungs.
It should be noted that in conjunction with the treatment of ankylosing spondylitis with stem cells, therapeutic exercises play a particularly important role. With ankylosing spondylitis, various bends, turns of the body in all directions, rotation of joints, etc. are fully used. Such energetic and high-amplitude movements should prevent the fusion of the vertebrae and the “ossification” of the spinal ligaments.
You need to exercise daily for at least 30-40 minutes. Moreover, it is advisable not to miss a single day! The patient must understand that every lost day gives the disease an irrevocable piece of a joint or a tiny piece of the spine, which becomes ossified and will never regain mobility!
According to reviews of the treatment of ankylosing spondylitis with stem cells, improvement is observed only in half of the cases and only at the initial stage of the disease.
Save on social networks:
Pathophysiology
Main article: Pyramid signs
It is a manifestation of damage to the central motor neuron system, which includes motor neurons of the precentral gyrus of the cerebral cortex, as well as their axons that make up the corticospinal tract (Latin tractus corticospinalis), going to the motor neurons of the anterior horns of the spinal cord.
Fibers of the corticospinal tract conduct inhibitory impulses that prevent the emergence of ontogenetically older segmental spinal reflexes. When the central motor neuron system is damaged, the flow of inhibitory impulses to the motor neurons of the spinal cord stops, which is particularly manifested by the occurrence of the pathological Rossolimo reflex.
It was noted that, in contrast to the pathological Babinsky reflex, which appears in acute damage to the pyramidal system (with the exception of spinal cord injury with the phenomenon of spinal shock), the Rossolimo reflex is a later manifestation of spastic paralysis.