Difficulties in making a diagnosis
Psychosis in children has nothing to do with loud crying and rolling on the floor, which almost every baby experiences from time to time. This mental disorder is characterized by a certain set of symptoms. To make this diagnosis, the patient must be examined by doctors of various specialties. Why is it so difficult to identify mental disorders in minors? The fact is that evidence of a violation of mental balance is problems with thinking and speech. Since these processes are poorly formed in young patients, it is difficult for the doctor to determine the nature of the deviation. The only diagnostic criterion will be behavior.
Experts are not sure that it is necessary to distinguish between psychosis in children and in people of puberty. Some doctors believe that adolescent mental disorders should be classified as a separate category. Their manifestations will differ from signs of behavioral abnormalities in children.
Another diagnostic difficulty is the similarity of symptoms of psychosis, hysterical personality traits and neuroses. In general, all mental disorders lead to a lack of adequate perception and difficulties in social life.
Psychosis - symptoms
In the lives of some people, sometimes grief occurs: someone from their family circle falls ill with psychosis, as a result of which the relative turns into a completely different person.
Psychosis - symptoms and treatment
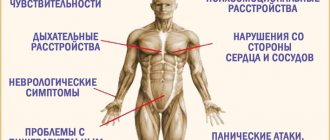
All types of psychosis have common symptoms such as:
- Affective reactions characterized by strangeness.
- Inappropriate behavior of the patient.
- Perception of reality that does not correspond to reality.
- Difficulties with perception of reality.
If psychosis occurs, you should consult a specialist. He must explain to the patient's relatives how to get rid of psychotic symptoms and, if necessary, prescribe medications to the patient.
Alcohol psychosis - symptoms
This type of psychosis is a disorder in a person’s mental activity, manifesting itself in the second and third stages of alcohol dependence.
The following types of alcopsychosis are distinguished:
- Alcoholic delirium (popularly known as “delirium tremens”). Symptoms: the desire for alcohol disappears, there are frequent mood swings, tremors in the limbs, the patient often has nightmares, suffers from insomnia, and hallucinations.
- Hallucinosis. Symptoms: auditory hallucinations, persecution mania, attacks on people (allegedly in order to prevent their aggression), decreased emotionality.
- Pseudoparalysis. Symptoms: mental degradation, delusions of grandeur appear, soon the patient shows passivity to the outside world, pain in the limbs appears.
- Encephalopathy. Symptoms: metabolic disorders. liver function, hypovitaminosis is observed.
Reactive psychosis and its symptoms
Reactive psychosis manifests itself as a result of the influence of factors that carry special significance or threaten the patient’s life. The main feature of this psychosis is that it disappears as soon as the causes of the problem are eliminated.
The main symptoms include:
- Excitement and inhibition (reactions with excitement are expressed by chaotic movements; with inhibition it is different: the patient falls into a stupor and cannot move).
- The behavior is accompanied by either loud laughter or sobs.
- Correct orientation in time and place is disrupted.
Depressive psychosis - symptoms
This disease occurs in the form of depressive attacks that occur intermittently. From them, the patient emerges personally whole, without any special changes.
- Depressed mood.
- Slowness in motor and mental processes.
- An oppressive feeling of hopelessness.
- A feeling of pinching in the region of the heart.
- Apathy towards loved ones.
- Sorrowful facial expression.
- Life, from the patient’s point of view, has no meaning; he sees no prospects for the future.
Psychosis in children and its symptoms
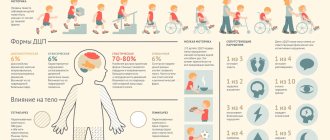
Childhood psychoses are a group of severe disorders. The most common are: childhood schizophrenia and childhood autism.
Common symptoms:
- There is a tendency of the patient to inflict any kind of injury on himself.
- Closedness. difficulty building interpersonal relationships.
- Interest in inanimate objects. Strange actions towards them on the part of a sick child.
- Speech disorders.
- Increased anxiety.
- Motor impairment.
Paranoid psychosis - symptoms
Is a delusional disorder. The main symptom is that the patient claims that they are trying very hard to influence him using magic, high-precision technology. Often, this psychosis is observed in schizophrenia.
Postpartum psychosis and its symptoms
The causes of this psychotic state are complications that arose during childbirth.
- Auditory hallucinations.
- Inadequate self-esteem.
- Thoughts about suicide, murder.
- Abnormal thinking. Inability to express oneself competently.
- Appetite disorder.
It is important to remember that the earlier psychosis is identified, the easier it will be to overcome it.
What factors contribute to the development of pathology?
Today experts do not have a clear answer to this question. But there is evidence that signs of psychosis in a child arise due to the following circumstances:
- Use of certain medications.
- Hormonal imbalances.
- Inflammation of the meninges.
- Infectious pathologies that are accompanied by a significant increase in temperature.
- Mechanical damage received during childbirth.
- Alcohol abuse by the mother during pregnancy and breastfeeding, taking medications.
- Mental stress, traumatic events.
- Poor heredity, manifestation of signs of mental disorders in one of the family members.
- Incorrect tendencies in upbringing (callousness, violence on both the physical and emotional levels).
This disorder can begin both in preschool and at a later age. As a rule, a pathology that was provoked by some factor (for example, a serious illness) goes away on its own after the symptoms of the underlying disease disappear. When the baby’s body is restored, mental balance also returns to normal. In some cases, psychosis in children occurs without the influence of environmental circumstances. Experts believe that this can be explained by biochemical disorders. They develop as a result of a difficult delivery, or the mother's use of alcohol or drugs. Unfavorable circumstances only provoke symptoms of mental disorders to which the patient was predisposed.
The most common mental disorders in children
Mental disorders in children are a unique group of diseases that are formed as a result of disturbances in emotional development.
These may include minor problems that can be easily corrected, as well as more serious processes that limit the life of the baby. The severity, reversibility and characteristics of the course of such an illness largely depend on the age characteristics of the baby and on the stage at which the problem was discovered. Often, mental disorders go unnoticed and untreated due to the inattention of parents or their fear of showing the child to a doctor. Subsequently, most of the phenomena are accompanied by registration with a psychiatrist or neurologist. Plus, all this is associated with a long period of treatment and long-term difficult rehabilitation, and this entails additional time expenditure for parents and the child himself. In fact, the sooner a disease is detected, the more quickly measures will be taken to treat it.
The list of ailments that are characterized by disorders of a child’s mental development is small and includes only 4 classes of deviations. Each of them involves certain variants of the course, causes and symptoms:
- mental retardation;
- early autism in children;
- ZPR;
- attention deficit syndrome.
Most often, these diseases are typical for preschool children. The sooner they are diagnosed, the greater the chance of complete relief from these pathologies. To do this, you need to know the description of each of them.
Signs of pathology
With psychosis in children, the following symptoms are observed:
- Hallucinations of a visual and auditory nature. The patient sees things, people, animals or events that are not really there. It can talk about sounds, touches or smells that are not present in the real world.
- Confused nature of consciousness. This symptom manifests itself during speech. The patient's statements are meaningless and unrelated to each other.
- Impulsive behavior. It can be unbridled joy, anger. The child gets irritated over trifles, breaks objects, and treats pets cruelly.
- Aggression towards people, both peers and adults. When visiting an educational institution, the patient calls his peers names and fights.
- Fluctuations in appetite. The child may constantly feel hungry, and after a while completely refuse food.
- Staying in the same position for a long time, poor facial expressions, a frozen or sad expression in the eyes.
- Lability of the emotional background. Apathy and sadness are replaced by excitement and anger.
- Strong manifestations of feelings. This symptom is expressed in loud crying, resentment, and attacks of fear.
- Sleep disturbances (increased activity at night, fatigue during the daytime).
- Constant pain in the head, fatigue for no particular reason.
- External signs of the disease (cold skin, profuse sweating, dry lips, increased pupil volume). Seeing such a patient gives the impression that he is suffering from fever.
Psychosis: what it is, symptoms, signs, treatment in women and men
Psychosis is a pathological process accompanied by a disturbance of the state of mind and a characteristic disorder of mental activity. The patient has a distortion of the real world, his memory, perception and thinking are impaired.
Online consultation on the disease “Psychosis”. Ask a question to the experts for free: Psychotherapist.
- Causes
- Manifestations
- Types of psychoses
- Postpartum
- Mass
- Paranoid
- Senile
- Alcoholic
- Reactive
- Spicy
- Schizoaffective
Briefly about the disease
For the most part, psychoses are endogenous, that is, the causes of their occurrence are internal. Due to heredity, schizophrenia, diseases of an affective nature (depressive disorders), and schizoaffective psychosis can occur.
Such diseases are the most severe and protracted.
It seems to us that the identification of psychosis and schizophrenia is not entirely correct, since the former can be observed in a large number of mental illnesses, such as epilepsy, Alzheimer's disease, alcoholism, dementia, mental retardation, etc.
A transient psychotic state can be provoked by taking medications or drugs, or it can be a psychogenic (reactive) psychosis, which is caused by severe mental trauma or shock (death of a relative or friend, threat to life).
Science also knows other types and causes of psychosis: the so-called infectious (a consequence of an infectious disease), somatogenic (the cause is severe somatic damage to organs), intoxication (for example, an alcoholic mental disorder called delirium tremens).
Psychoses are very common disorders of consciousness. Thus, endogenous psychoses are diagnosed in approximately 5% of the population. But since different countries have adopted different approaches to defining such diseases, which are often very difficult to diagnose, statistical data differ.
We also do not have accurate data on how many people suffer from exogenous psychotic disorders (those of external origin).
This is understandable: most of these pathologies occur in drug addicts and alcoholics. The manifestations of psychosis reflect the boundless richness and versatility of the human psyche.
Therefore, we can indicate only the most common manifestations:
- Hallucinations. First of all, they are divided into auditory, optical, olfactory, gustatory and tactile - depending on the analyzer. Hallucinations are also divided into simple (noise, calling) and complex (speech). Most often, these are voices heard by a person and emanating either from the outside world or from the patient’s head. They are so natural that the patient has no doubt about their reality. The following danger is associated with this. Because they can threaten, accuse, or command, a person perceives them either as a call to action (the patient, by obeying, may harm himself or those around him) or as an emotional assessment, which can aggravate a mental disorder.
- Crazy ideas. These are thoughts and conclusions that do not correspond to the state of things in the real world. They completely take over a person’s consciousness, and there is no way to convince him, explain the situation, or correct this condition. Such ideas are varied, but most often they are like this:
- delusion of persecution - the patient believes that he is being watched in order to harm him in one way or another: to kill, defame, involve him in an adventure or conspiracy;
- delusion of influence - the patient believes that he is influenced by psychics, aliens, radiation from intelligence equipment, radiation, black magic, witchcraft, induced damage;
- delusion of damage - the patient thinks that they are trying to poison him, that things are being stolen from him, that they are being taken out of the house;
- hypochondriacal delusion - the patient diagnoses himself with a very serious illness, often fatal, and does not believe the doctors who convince him that he is completely healthy.
In addition, delusions of jealousy, uniqueness, invention, foreignness, greatness, love, reformation and others are described.
- Movement disorders. In this case, the patient is either inhibited (in a stupor) or too excited. In the first case, he moves little, often freezes in some position, does not eat, and his gaze is riveted to one point. If the patient is subject to psychomotor agitation, he continuously talks, moves, makes grimaces, teases people; in his actions he is subject to impulse and momentary desires, and then cannot explain his actions.
- Mood disorders, the manifestations of which are depressive and manic states. In case of depression, the patient’s mood worsens, a melancholy feeling occurs, depression occurs, movements are inhibited, intellectual activity decreases, the desire to do anything disappears, the person is consumed by pessimism, and suicidal thoughts appear. If a person is in a manic state, then the mood is unmotivatedly high, muscle activity increases, mental activity accelerates, inflated self-esteem appears, unrealistic, even fantastic plans appear, the need for sleep disappears, but all desires are disinhibited, and the patient may begin to abuse alcohol or drugs , have sexual relations with many partners.
These are so-called positive disorders, which got their name due to the fact that these symptoms seem to be added to the mental state of the patient, as it was before the illness.
Often, even after the symptoms of psychosis have completely disappeared, the patient begins to experience disorders called negative ones - in many cases they cause very serious social consequences than the psychotic state itself.
Such disorders received such a definition due to the fact that a person’s character, basic personality traits, and huge layers simply disappear from the psyche. Such people lose initiative and are lethargic and passive in most life situations.
It is often noted that the energy tone is significantly reduced, desires and the desire to perform any actions disappear, emotional dullness increases, the person seems to be fenced off from society, breaking off all contacts with other people.
Often the former responsiveness, tactfulness, and sincerity are replaced by previously uncharacteristic anger, rudeness, and an unwillingness to coexist peacefully with loved ones. Thinking also undergoes serious changes: it becomes amorphous and loses its content.
Such conditions in many cases lead to loss of ability to work and, consequently, to disability.
Psychosis in children aged 1 year
Mental disorders are very difficult to detect in infants. Deviations can be suspected if there are autistic tendencies in behavior. The baby does not smile, he does not show emotions. The development of the speech process is delayed. Obsessive actions (for example, clapping hands) are observed. The baby is not interested in surrounding objects and does not show affection for relatives. As patients with this disorder get older, diagnosing psychosis in children is not such a difficult task for specialists.
Symptoms depending on the form of failure
Different symptoms of mental illness are justified by different forms of the disease. Common symptoms of the disease are:
- hallucinations - the baby sees, hears, feels something that is not really there;
- delusion – a person sees the existing situation in his own incorrect interpretation;
- decreased clarity of consciousness, difficulty in orientation in space;
- passivity, lack of initiative;
- aggressiveness, irritability, rudeness;
- obsession syndrome.
- deviations associated with thinking.
Psychogenic shock often occurs in children and adolescents. Reactive psychosis occurs as a result of psychological trauma.
This form of psychosis has signs and symptoms that distinguish it from other mental spectrum disorders in children:
- its reason is deep emotional shock;
- reversibility - symptoms weaken over time;
- symptoms depend on the nature of the injury.
Early age
At an early age, mental health problems manifest themselves in autistic behavior in the child. The baby does not smile or in any way show joy on his face. Up to a year, the disorder is detected in the absence of humming, babbling, and clapping. The baby does not react to objects, people, or parents.
Age crises, during which children are most susceptible to mental disorders from 3 to 4 years, from 5 to 7, from 12 to 18 years.
Early mental disorders manifest themselves in:
- frustration;
- capriciousness, disobedience;
- increased fatigue;
- irritability;
- lack of communication;
- lack of emotional contact.
Later ages up to adolescence
Mental problems in a 5-year-old child should worry parents if the child loses already acquired skills, communicates little, does not want to play role-playing games, and does not take care of his appearance.
At the age of 7, the child becomes mentally unstable, he has an appetite disorder, unnecessary fears appear, his performance decreases, and rapid fatigue appears.
At the age of 12-18, parents need to pay attention to their teenager if he or she develops:
- sudden mood swings;
- melancholy, anxiety;
- aggressiveness, conflict;
- negativism, inconsistency;
- a combination of the incompatible: irritability with acute shyness, sensitivity with callousness, the desire for complete independence with the desire to always be close to mom;
- schizoid;
- refusal of accepted rules;
- penchant for philosophy and extreme positions;
- intolerance of guardianship.
More painful signs of psychosis in older children include:
- suicide attempts or self-harm;
- causeless fear, which is accompanied by palpitations and rapid breathing;
- desire to harm someone, cruelty towards others;
- refusal to eat, taking laxative pills, strong desire to lose weight;
- increased feeling of anxiety that interferes with life;
- inability to persevere;
- taking drugs or alcohol;
- constant mood swings;
- bad behavior.
Onset of mental disorder at age two
As a rule, this condition is associated with the influence of provoking factors. Such circumstances include various infectious pathologies, use of medications, high fever, poor functioning of the immune system or lack of nutrients. Genetics plays an important role. The course of psychosis in a 2-year-old child can be acute, and it occurs suddenly and clearly manifests itself. Sometimes the disease is protracted or periodically provokes a worsening of the condition.
According to reviews, in some cases the pathology makes itself felt over a long time.
In two-year-old patients, psychosis can be suspected in the presence of apathy, sleep disturbances, refusal to eat, attacks of pain in the head and palpitations. Since the illness is often associated with physical illnesses, the child should be examined by specialists of various profiles. For example, you need to check how correctly the organs of vision are working, and whether the baby has hearing or speech impairments.
Diagnosis of psychosis in a child
In case of progression of mental retardation, the child’s personality is extremely immature, and the psyche develops at a very slow pace. The cognitive sphere, as well as the behavioral reaction, is impaired. When establishing a prognosis, it is worth paying special attention to the causes of the disease, as well as paying attention to some signs of pathology.
It is important to organize training and educational activities in a timely manner, which will smooth out the main symptoms of the disease and bring the child’s health to normal. It is especially important to provide comprehensive rehabilitation and involve several specialists in the treatment process at once - a speech therapist, a psychiatrist, a pediatrician. Daily homework behavior with parents plays an important role for the overall development of the baby.
Mental illnesses in children are of an unexplored nature, so it is problematic to name the exact causes of their occurrence. However, there are several factors that increase the likelihood of developing neuropsychiatric disorders in children.
These disorders are:
- congenital diseases of the brain and central nervous system;
- complex pathological pregnancy or damage during childbirth;
- genetic predisposition and hereditary factors;
- unfavorable microclimate in the family in which the child is growing up;
- the presence of acute and chronic pathologies in parents;
- injuries;
- lack of proper attention given to the child.
As you can see, the causes can be very different. If these factors are present (as well as if any manifestations of the disease are detected in the child), parents should show the baby to the doctor.
There are a large number of diagnostic techniques that will help explain the manifestation of certain symptoms of mental disorders in children.
The target function of the PMPC is an integrated approach to studying the child’s health status, provided by several specialists. This group includes a social worker, psychologist, neurologist, psychiatrist, speech pathologist, speech therapist, and nurse. During the activities, the history of the young patient is carefully studied, and appropriate conclusions are made.
Survey
This is an important stage in the overall mechanism of helping a child with certain mental developmental disabilities. However, in practice, due to the lack of a comprehensive analysis in the presence of such diseases, the task is not completely fulfilled. This factor negatively affects the further therapeutic process.
This event, first of all, includes an examination to collect anamnestic data, as well as to assess the neurological, mental and somatic condition of the baby. The goal is to evaluate the nervous system and find ways to influence it in case of abnormalities.
Mental analysis
This method involves paying attention to the living conditions and upbringing of the baby, as well as the nature of communication. The study of this functionality always implies taking into account the age characteristics and development of the child as a whole. At the same time, an assessment is made of the state of attention, perception, memory, and intellectual picture.
Childhood psychosis is a complex mental illness characterized by a distorted perception of reality, expressed in the inability to separate fantasy from fiction. The child tends to give inadequate reactions to some everyday situations, which makes his daily life difficult. When organizing their thinking, such children experience a breakdown; it becomes more difficult for them to control their actions, fit them into generally accepted standards, make adequate decisions and speak competently. Psychosis among children is quite rare. They are divided into early (infants, preschoolers and schoolchildren) and late stages (adolescents).
A variety of factors can be prerequisites for the onset of childhood psychosis:
- use of medications;
- heat;
- hormonal imbalances;
- meningitis;
- birth injuries;
- alcohol intoxication;
- severe stress, psychological trauma;
- congenital characteristics and malformations of the body.
When the physical cause of the disease (stress, for example) is eliminated, it disappears safely. This may take some time - on average, 1-2 weeks, during which the child adapts to the conditions of real life.
Psychosis can act as an independent disease and occur separately from other diseases. This situation is typical for child health problems due to childbirth, uncontrolled medication use, and alcohol poisoning.
Children with congenital abnormalities in physical development often experience psychosis, even in early childhood.
There is an opinion that the external characteristics of a child’s behavior do not always necessarily indicate the presence of psychosis if it occurred at an early age of the child and was symptomatic. Researchers prefer to rely on data on the genetic nature of this phenomenon.
The causes of psychosis can be short-term or long-term physical conditions. These include taking medications, high fever, hormonal imbalance, and meningitis. Typically, an attack of psychosis, the source of which is a physical problem, stops with its solution.
There are cases of the development of psychosis in children without the presence of concomitant diseases. There is an expert assumption that the source of such conditions is a deviation of a biochemical nature. These deviations are considered to be acquired during childbirth or acquired after malicious use of drugs or alcohol.
Children born with severe constitutional disorders suffer from psychoses that spontaneously manifest at an early age. They typically remain disabled throughout their lives. Many doctors do not consider external factors to be convincing for psychosis if it manifests itself symptomatically in early childhood. Research is testing the theory of a genetic factor as the source of the disease.
Diagnostic measures for suspected psychosis in a child take several weeks or months. He should be carefully examined by the following doctors: a specialist in developmental diseases, an otolaryngologist, a speech therapist, a neurologist. A physical and psychological examination is carried out - the child’s behavior is observed for a long time, mental abilities are tested, hearing and speech are checked. Hospitalization is possible for various types of studies of the nervous system.
If it is determined that a child's psychosis is based on a physical illness, the diagnosis switches to searching for its cause. Parents always have the right to doubt the correct diagnosis and can get advice from other specialists.
Manifestations at three years of age
The disease is characterized by deviations in behavior and lack of logic in statements. The patient does strange things. Psychosis in a 3-year-old child can also be suspected if there are sudden mood changes. The patient's reactions to external circumstances are inadequate. For example, he may get angry at a harmless remark, invent new words, or laugh in a situation when he should be sad. In addition, the child sees or feels something that is not there.
Sometimes it is difficult for parents to distinguish fantasies from hallucinations of various types. Naturally, the boy can play the prince who saves the beauty from the dragon. However, if the patient does see a monster, he experiences strong emotions, such as intense fear, and behaves accordingly.
Attacks of mania and depression in a child
This condition is extremely rare in minors. Before adolescence, pathology is difficult to identify due to the absence of symptoms. Most often, the disease manifests itself during puberty due to changes in the balance of hormones.
Manic-depressive psychosis in children can develop under the influence of the following reasons:
- Bad heredity.
- Age of mother and father (the older the parents, the higher the likelihood of pathology).
- Sleep disorders.
- Mental stress, stressful situations.
- Infectious pathologies.
Children with this disease do not show signs of mania. But there are such deviations as:
- Increased activity.
- Excessive cheerfulness.
- Early interest in sex.
- Aggression.
- Excitation.
Such symptoms are present for a certain time, and then are replaced by others:
- Feeling overwhelmed, lethargic.
- Increased sleepiness.
- Discomfort in different parts of the body. In this case, the patient cannot indicate the location of the unpleasant sensations.
- Insomnia.
- Fears.
- Whims, refusal to play activities.
- Suicidal tendencies.
Psychotic. Manifestation and treatment of various forms of psychosis in children Infantile psychosis in children
Psychoticforms of autism (infantile psychosis and endogenous atypical childhood psychosis) must also be differentiated. The possibility of separating these two types of psychoses is clearly confirmed by significant differences in clinical parameters. Similar in disintegrative dissociated dysontogenesis and the presence of catatonic disorders in attacks, they differ not so much in the time of manifestation of the disease [Bashina V.M., 1999; 2009], how many by the presence or absence of regression in attacks, stereotypies in remission, duration of manifest attacks, outcomes [Simashkova N.V., 2011; Garralda ME, Raynaud JP, 2012]. The catatonic syndrome in IP occupies the main place in the structure of the attack and is replaced by the acquired hyperkinetic syndrome - in remission. Catatonic disorders in ADP occur as a continuous syndrome in an attack, remission, and throughout life in the form of protopathic motor stereotypies. IP is characterized by a positive dynamics of the course of the disease, a favorable outcome – in 84% [“practical recovery” – in 6%; “high-functioning autism” (not to be confused with Asperger’s syndrome) – 50%; regressive course – in 28%]. Endogenous ADP is characterized by a progressive course of the disease with early formation of cognitive deficit in 80% of cases (Table 2).
The functional characteristics of the central nervous system, assessed by neurophysiological parameters, also differ significantly in these diseases. There is a correlation between the severity of the clinical picture and the degree of EEG disturbance. In clinical EEG, a negative effect on the bioelectrical activity of the brain is considered to be a decrease in the power of the alpha rhythm and an increase in the power of slow rhythms of the theta-delta ranges. Teta-ri for severe diseases with the collapse of higher mental functions and for sick children with significant developmental delays. With endogenous ADP, there is a correlation between the quantitative measure of the theta rhythm and the clinical manifestation of regression - as the condition improves, its severity decreases. In patients of this group, the theta rhythm, as a rule, persists for a long time (coincides with the presence of motor stereotypies in the clinical picture of the disease), which confirms an unfavorable prognosis.
Table 2. Clinical differentiation of psychotic forms of ASD
Infantile psychosis
| Atypical childhood psychosis | ||
| Dysontogenesis | Dissociated dysontogenesis | Autistic disintegrative dysontogenesis |
| Catatonic syndrome | Catatonic syndrome with acquired hyperkinetic syndrome in remission and subsequently stops | Catatonic disorders in ADP in manifest attacks are combined with regressive ones and persist throughout life in the form of motor stereotypies |
| Flow | Positive dynamics during the course of the disease | Progressive course with early formation of cognitive deficit, schizis, anhedonia, alexithymia in 80% |
| Exodus | Favorable: in 6% - “practical recovery”, in 50% - “high-functioning autism”, in 44% - regressive course with mitigation of autism | Unfavorable in 80%: severe autism, oligophrenia-like defect persists |
The milder psychotic form of ASD - IP with catatonic disorders is characterized by the absence of the theta rhythm and the presence of a regular alpha rhythm in the attack, which is prognostically favorable.
An additional marker of this disease can be a pronounced sensorimotor rhythm, which appears during the period of remission, when catatonic disorders are replaced by an acquired hyperkinetic syndrome. According to pathopsychological studies, ADP and IP have different outcomes of cognitive impairment: preservation of stable cognitive deficit in ADP and partial leveling of cognitive dysontogenesis against the background of habilitation in IP.
Atypical childhood psychosis of endogenous origin should be differentiated from syndromic ADP. Based on the behavioral phenotype at the height of a regressive-catatonic attack, it is difficult to distinguish patients with endogenous ADP from patients with syndromic psychotic forms of ADP (with Martin-Bell, Down, Rett syndromes, etc.). These psychoses have a phenotypically similar clinical picture in different nosologies: a general sequence of changes in stages in attacks (autistic - regressive - catatonic), unfavorable outcome. To clarify syndromic pathology, patients with regressive-catatonic psychosis need molecular genetic studies. In patients with syndromic forms of ASD, certain EEG patterns with dominance of rhythmic theta activity at certain stages of the disease have been identified (Gorbachevskaya N.L., 1999, 2011; Yakupova L.P., 2005). As mentioned above, the same pattern was recorded during EEG studies of endogenous ADP in the regression stage (Yakupova L.P., Simashkova N.V., Bashina V.M., 2006). The decrease in regressive manifestations during therapy was accompanied by a partial reduction of the theta rhythm and restoration of the alpha rhythm. This distinguishes endogenous ADP from severe syndromic forms of ADP, in which the alpha rhythm was practically not recorded.
Atypical autism (AA) or “mental retardation with autism features” in selected genetic syndromes (Martin-Bell, Down, Williams, Angelman, Sotos, etc.), diseases of metabolic origin (phenylketonuria, tuberous sclerosis, etc.) should be differentiated from the syndrome Kanner, in which severe autism persists throughout life, cognitive deficits increase. Motor stereotypies in syndromic forms of AA are phenotypically different. In non-psychotic forms of UMO with autistic features, sick children and adolescents have less or no disturbance in their emotional relationship with the world around them. In patients with syndromic forms of AA, epiactivity is observed in 20-30% of cases.
Differential diagnosis of ASD with other nosologies requires a careful study of the anamnesis, identification of the leading syndrome, and follow-up observation in order to clarify the nature of the course of the disease. ASD should be differentiated primarily from early-onset childhood schizophrenia (CS),
in which dissociated disintegrative mental development, socialization disorders, and stereotypies are also noted. The childhood form of schizophrenia (DS) is not mentioned in ICD-10 (1994). In the USA, childhood schizophrenia is extremely rarely diagnosed before the age of 14, in European countries - before the age of 9. During the adaptation of ICD-10 in the Russian Federation (1999), a special section was introduced - “schizophrenia (children’s type)” - F20.8xx3. It included severe forms of schizophrenia (catatonic, hebephrenic, paranoid) with a progressive, malignant course of the disease.
Typical symptoms of ASD differ from DS, but overlap with it. Genetic studies have shown an increased incidence of schizophrenia and other psychotic disorders in parents whose children have ASD. It remains controversial whether the "early childhood catatonia" described by Leonhard is the first manifestation of schizophrenia or a form of atypical autism. The DSM-V (2013) identifies catatonia, comorbid with mental disorders: schizophrenia, ASD, bipolar, depressive disorders, etc.
In addition, recently in Russia and a number of European countries, endogenous atypical childhood psychosis has been identified among autism spectrum disorders (Bashina V.M., 2009; Simashkova N.V. et al., 2006,2013; Garralda ME, Raynaud JP, 2012 ; Meyer-Lindenberg A., 2011), occupying 8-12% of the spectrum of autistic disorders. It includes regressive forms of autism with comorbid catatonic symptoms and with the early formation of an oligophrenic defect. It is difficult to distinguish between these forms of atypical autism and childhood schizophrenia. Biological markers identified in recent years, along with clinical and pathopsychological ones, can make a significant contribution to solving diagnostic issues, differentiating the selection of individual therapy, and monitoring the condition of patients.
ASD
should be differentiated from
defects of the sensory organs (vision and hearing) and mental retardation (MRD).
In the latter, uniform total underdevelopment should be noted in the first place. In cases of mental illness with autistic features in children and adolescents, the emotional relationship to animate or inanimate objects of the surrounding world is to a lesser extent disturbed or not at all disturbed. Motor disorders in the form of stereotypies have their own characteristics and differ from motor stereotypies in childhood autism.
ASD
must be distinguished from
deprivation syndrome
, attachment disorders as a result of severe pedagogical neglect. These children may also have impaired ability to communicate, but more often in the form of depressive symptoms. Sometimes there is no distance in behavior, but there is no typical ASD triad.
When discussing the presence of comorbidity of ASD with organic diseases of the brain (epilepsy, residual manifestations of early organic damage to the central nervous system of perinatal origin, encephalopathy, brain injuries, etc.), we should dwell on the concept of the pathogenesis of autism, which has become popular in recent years among neurologists due to non-convulsive epileptic encephalopathy. With this form of epilepsy, cognitive, autistic and other mental development disorders are noted (Zenkov et al., 2004; Zenkov, 2007; 2008; Mukhin et al., 2011; Tuchman & Rapin, 1997; Chez & Buchanon, 1997; Kim et al. , 2006; Berney, 2000). The EEG of such patients reveals pronounced epileptiform activity (electrical status epileptiform) mainly during the slow-wave stage of sleep, but no clinical picture of attacks is observed. It is believed that the epileptiform activity detected in these cases is associated with congenital disorders of brain maturation processes (Doose, 1989, 2003; Mukhin et al., 2011). It is argued that it is after the appearance of epi-activity in a certain period of ontogenesis that a significant regression occurs in the cognitive and mental spheres, which is called autistic epileptiform regression (Canitano, 2006; Characteristics of developmental regression in autistic children, 2010). This theory is supported by facts confirming that treatment of non-convulsive encephalopathies with anticonvulsants leads to a noticeable improvement in the condition of patients, and this resolves the issue of causal treatment of ASD (Zenkov et al., 2004; Zenkov, 2007; Mukhin et al., 2011; Lewine et al. al., 1999). However, the cause-and-effect relationship of events proposed in the above concept cannot be considered convincingly proven for all forms of ASD. For example, in Rett syndrome, autistic disorders appear much earlier than epileptic activity.
Discussing the question of whether there is a connection between epilepsy and autism, A. Berg and Plioplys (2012) emphasize that such a connection is observed with cognitive impairment, when it is significantly expressed in children with epilepsy or autism. In cases where intellectual impairment is not present, there is little evidence of the risk of autism in children with epilepsy. To this we can add that in severe forms of UMO (for example, with Rett syndrome), the severity of autism is greater in those patients who have fewer neurological disorders (including epi-activity). Is epilepsy comorbid with autism, is it caused by autism, or does epilepsy itself lead to the development of ASD? It is difficult to answer these questions unambiguously at the current stage of scientific development, and therefore the question of the relationship between different forms of autism spectrum disorders and epilepsy cannot yet be considered resolved.
HABILITATION
It is necessary to adhere to a unified preventive-therapeutic approach in the treatment of patients with ASD, the goal of which is the overall development of children, adolescents and adults suffering from autism. The integrated use of drug and non-drug treatment methods (defectological, psychological, pedagogical, neuropsychological correction, psychotherapeutic social work with the patient and his family) is one of the fundamental principles of the supervision of autistic disorders in children. Habilitation efforts are aimed at relieving positive symptoms of the disease, reducing cognitive impairment, mitigating the severity of autism, social interaction, stimulating the development of functional systems, and creating the prerequisites for learning opportunities. Depending on the leading cause of the increase in behavioral disorders, the structure of therapeutic measures shifts towards either predominantly drug therapy or strengthening the correctional, pedagogical and psychotherapeutic components of complex treatment.
Main areas of treatment:
Impact on the pathogenetic mechanisms of disease development;
Activation of the patient’s biological and psychological capabilities;
Impact on comorbid mental and somatoneurological disorders.
Principles of therapy:
A personalized approach taking into account the established or suspected etiology, all links of pathogenesis, clinical components of the disease, the presence of additional comorbid disorders in relation to autism;
Integrated use of drug and non-drug treatment methods;
“multimodality” with the participation of a team of specialists: psychiatrists, pediatricians, neurologists, psychologists, speech pathologists, teachers, social workers.
PSYCHOPHARMACOTHERAPY
Early initiation of drug therapy is important as a favorable prognostic factor. This is due to the patterns of brain development and positive trends in ontogenesis when the active course of the disease is stopped.
For different types of ASD, drug therapy is radically different. In addition, drug therapy is indispensable under the influence of external and internal unfavorable factors (changes in the environment, microsocial environment, critical periods of development). Drug correction is necessarily combined with developmental education, the principles of which will be outlined below. There is a correlation between the age of onset of therapeutic and corrective interventions and clinical and social prognosis
for patients with autism.
To prevent the formation of severe personality and oligophrenia-like defects, early and adequate preventive measures are necessary.
Treatment is carried out taking into account the psychopathological structure of the exacerbation of the disease, which determines the choice of psychotropic drugs, as well as taking into account the characteristics of the therapeutic or spontaneous transformation of the syndrome during the treatment process, which may be associated with the replacement or addition of other treatment methods. The choice of a specific drug is carried out taking into account the spectrum of psychotropic activity of the antipsychotic and the nature of the side effects that occur, as well as contraindications for use and possible drug interactions. The dosage regimen, average and maximum permissible daily doses and the possible route of administration of a particular antipsychotic are determined by the nature and severity of the existing psychopathological symptoms, the somatic condition and age of the patient. Polypromasia should be avoided. The effectiveness of the therapy is assessed based on the positive dynamics of clinical manifestations. The main indicators are the speed of development and durability of the effect, as well as the safety of therapy.
In the case of the development of acute psychosis with a predominance of nonspecific autistic manifestations (phobias, anxiety, psychomotor agitation, aggressiveness), one should resort to prescribing antipsychotics with a sedative component of action (chlorpromazine, levomepromazine, chlorprothixene, alimemazine, periciazine, etc.), including parenterally (the strength of the evidence IN).
Disinhibiting antipsychotics (sulpiride) are prescribed taking into account their disinhibiting, activating effect (strength of evidence B).
Polymorphism of psychopathological disorders, the presence of symptoms of deeper registers requires the prescription of antipsychotics with a powerful general antipsychotic (incisive) effect (haloperidol, clozapine, risperidone).
Pharmacokinetics
There is accurate data on the mechanisms of action of drugs. An important task for medical professionals involved in autistic disorders (mainly child and adolescent psychiatrists) is to disseminate this knowledge among doctors and other related professionals, as well as among parents. Persistent prejudice against drug treatment does not improve the condition of patients with autism.
The antipsychotic effect of neuroleptics is associated primarily with blockade of D2-dopamine receptors and changes in dopaminergic neurotransmission, which in turn can cause extrapyramidal disorders and hyperprolactinemia. The development of certain clinical effects of D2 receptor blockade depends on the effect on various dopaminergic pathways in the central nervous system. Inhibition of neurotransmission in the mesolimbic system is responsible for the development of the antipsychotic effect itself, in the nigrostriatal region - for extrapyramidal side effects (neuroleptic pseudoparkinsonism), and in the tuberoinfundibular zone - for neuroendocrine disorders, including hyperprolactinemia. In mesocortical structures in patients with autism, a decrease in dopaminergic activity is observed. Antipsychotic drugs bind to D2 receptors differently in different brain structures. Some substances have strong affinity and block receptors for a long time, while others, on the contrary, are quickly released from binding sites. If this occurs at the level of the nigrostriatal region and the blockade of D2 receptors does not exceed 70%, then extrapyramidal side effects (parkinsonism, dystonia, akathisia) either do not develop or are only slightly expressed. Antipsychotics with anticholinergic activity are less likely to cause extrapyramidal symptoms, since the cholinergic and dopaminergic systems are in a reciprocal relationship, and blockade of type I muscarinic receptors leads to activation of dopaminergic transmission. The ability of central anticholinergic drugs (trihexyphenidyl, biperiden) to correct neuroleptic extrapyramidal disorders is based on the same mechanism of action. Some drugs, depending on the dose used, are able to block presynaptic D2/3 receptors and paradoxically facilitate dopaminergic neurotransmission, including at the cortical level (sulpiride). In the clinic, this can manifest itself as a disinhibiting or activating effect.
Atypical antipsychotics (type 2 neuroleptics) can also block 5-HT2 serotonin receptors, which is associated with their ability to reduce the severity of negative symptoms and cognitive impairment in patients with autistic disorders, since type 2 serotonin receptors are located predominantly in the cerebral cortex (especially in the frontal areas ) and their blockade leads to indirect stimulation of dopaminergic transmission. The prescription of atypical antipsychotics in the treatment of ASD in childhood requires the simultaneous administration of central anticholinergic drugs (trihexyphenidyl, biperiden).
Currently, there are significant age restrictions when prescribing antipsychotics. Taking into account the constant work of various structures to introduce modern drugs into child psychiatric practice, age restrictions on successfully used drugs in adults are gradually being lifted. When choosing a drug, you should also be guided by the current state of psychiatry and the recommendations of manufacturers in accordance with the laws of the Russian Federation.
The following groups of antipsychotics are used to treat psychotic forms of ASD:
1. Phenothiazines and other tricyclic derivatives:
- Aliphatic (alimemazine, promazine, chlorpromazine)
- Piperidines (pericyazine, pipothiazine, thioridazine)
- Piperazine (perphenazine, thioproperazine, trifluoperazine)
2. Thioxanthenes (flupenthixol, chlorprothixene)
3. Butyrophenones (haloperidol)
4. Substituted benzamides (sulpiride, tiapride)
5. Dibenzodiazepine derivatives (clozapine)
6. Benzisoxazole derivatives (risperidone)
Aliphatic phenothiazines have strong adrenolytic and anticholinergic activity, which is clinically manifested by a pronounced sedative effect and a mild effect on the extrapyramidal system. Piperazine phenothiazines and butyrophenones have weak adrenolytic and cholinolytic, but strong dopamine-blocking properties, i.e. the most pronounced global antipsychotic effect and significant extrapyramidal and neuroendocrine side effects. Piperidine phenothiazines, thioxanthenes and benzamides occupy an intermediate position and have predominantly moderate antipsychotic effects and moderate or mild extrapyramidal and neuroendocrine side effects. A separate group consists of atypical antipsychotics (risperidone, clozapine), which have a fairly pronounced general antipsychotic effect and dose-dependent extrapyramidal and neuroendocrine side effects, which requires the simultaneous administration of central anticholinergic drugs.
The most commonly used antipsychotics and other medications in patients with ASD
When choosing a drug, you should be guided by the list of registered medicines approved for use in children and the recommendations of manufacturing companies in accordance with the laws of the Russian Federation (see Table No. 3-8).
Table 3.
The most commonly used antipsychotics in patients with ASD
| International nonproprietary name | Age of permitted use |
| Alimemazine, tab. | From 6 years old |
| Haloperidol, drops | from 3 years |
| Haloperidol, tab. | from 3 years |
| Clopixol | children's age, no exact data |
| Clozapine, tab. | from 5 years old |
| Levomepromazine, tab. | from 12 years old |
| Periciazine, caps. | from 10 years old, with caution |
| Periciazine, drops | from 3 years old |
| Perphenazine | over 12 years old |
| Risperidone, oral solution | from 5 years old |
| Risperidone, tab. | from 15 years old |
| Sulpiride | from 6 years old |
| Trifluoperazine | over 3 years old, with caution |
| Chlorpromazine, tablet, dragee |
Consequences of mental illness
This pathology does not pose a direct threat to life. However, its complications can be very unpleasant. Reviews indicate that the child becomes detached, uncommunicative, aggressive, his character deteriorates, and intellectual activity is impaired. Sometimes parents attribute changes in behavior to crises that go away on their own. However, such deviations are not as harmless as they might seem. Psychosis in a child 5 years of age and older has a bad effect on interaction with peers in educational institutions (in kindergarten, at school).
Outbursts of anger and uncontrollable reactions make it difficult to interact with others.
Therapy
For psychosis in children, treatment depends on the cause of the disorder, the symptoms and their severity. Often such deviations develop in minor patients under the influence of traumatic events. In this case, the pathology disappears on its own. The more time passes from the moment the stress factor appears, the better the patient’s condition becomes. In such cases, sessions with a psychologist and the creation of a calm environment help. If a mental disorder is caused by a physical pathology, the doctor should pay attention to the treatment of the underlying illness. Medicines are prescribed only in situations where the patient is angry.
Types of psychotic disorders among children
Children's mental illnesses are divided according to certain criteria. Depending on age, there are:
- early psychosis;
- late psychosis.
The first type includes patients with mental disorders of infancy (up to one year), preschool (from 2 to 6 years) and early school age (from 6-8). The second type includes patients of pre-adolescence (8-11) and adolescence (12-15).
Depending on the cause of the disease, psychosis can be:
- exogenous – disorders caused by exposure to external factors;
- endogenous – disorders provoked by the internal characteristics of the body.
Depending on the type of course, psychoses can be:
- reactive, which arose as a result of prolonged psychological trauma;
- acute – arising instantly and unexpectedly.
A type of psychotic disorder is affective disorder. Depending on the nature of the course and symptoms of affect disorders, there are:
- depressed;
- manic;
- schizoaffective;
- organic.