Stroke is a very dangerous disease that often leads to the patient’s disability or even death. Coma after a stroke occurs when there is extensive damage to brain cells due to an ischemic or hemorrhagic stroke.
Rupture of the vessel walls due to a sharp increase in blood pressure leads to hemorrhage in the brain tissue, and under the influence of the mass of blood in the affected areas of the brain, compression occurs, causing necrosis of these areas, increased pressure and severe swelling of the membranes of the brain.
With an ischemic stroke, coma occurs only when there is extensive damage to brain cells that do not receive oxygen; in milder cases, this dangerous complication can be avoided, or, as a result of a set of resuscitation measures, the patient can be quickly removed from a dangerous state.
Why does coma occur after a stroke and why is it dangerous?
Cerebral coma, which appears during a stroke, is a serious condition of the patient, bordering between life and death. It provokes a total disruption of the brain with further disruptions in the performance of all body systems during cerebrovascular disease. In most situations, a coma occurs due to apoplexy, characterized by hemorrhage in the brain. The following external factors can also affect the appearance of coma:
- sudden jumps in blood pressure;
- hormonal disorders and diseases leading to cerebral edema;
- ischemic disease of internal organs;
- intoxication of the body due to the breakdown of its tissues;
- atherosclerotic plaques on the vascular walls of the brain (atheroma);
- collagenosis;
- severe vitamin deficiency;
- accumulations of beta-amyloid in cerebral vessels;
- blood diseases.
Most often, the patient falls into a coma suddenly and in a short period of time - 15-30 minutes. In rare situations, over a long period (several days), obvious symptoms of a stroke are observed, when the patient slowly sinks into a severe coma. In this position, the person is unconsciously in deep sleep and practically does not react to various stimuli, but he is still alive and is often able to reanimate.
IMPORTANT!
Some patients with coma may respond to light by opening their eyes or spontaneously moving their limbs or whole body. Conversational functions are completely excluded, but sometimes emotional reactions appear in the form of grimaces, laughter, and crying.
A person in a coma is rarely able to survive it on his own, which is why he must be in the clinic under the constant supervision of the medical staff involved in his treatment. This pathological condition progresses rapidly and in most cases leads to the death of the patient, especially if it lasts more than 3 days and is accompanied by oxygen starvation of brain cells. The risk of death is indicated by the following factors:
- repeated stroke, resulting in a coma;
- complete lack of response to all external stimuli;
- extensive area of damage to blood vessels and brain tissue;
- old age of the patient - 70 years and older;
- critically low concentration of serum creatinine in the body;
- progressive necrosis of brain cells.
ATTENTION!
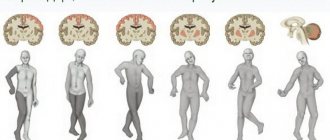
If the body actively fights and emerges from a cerebral coma, the patient often suffers from its consequences - memory gaps, attention and concentration disorders, although he does not always lose his physical abilities and is able to live normally. In many cases, varying degrees of disability are diagnosed and the need for treatment for the rest of the person’s life.
What is coma?
In December 1999, a nurse was straightening the sheets under a patient when she suddenly sat up and exclaimed, “Don’t do that!” While this is nothing unusual, it was a surprise to the patient's friends and family - Patricia White Bull had been in a deep coma for 16 years. Doctors told family and friends she would never come out of it.
How can a person come out of a coma after being in it for so long? What causes people to fall into a coma in the first place? What is the difference between being in a coma and being in a vegetative state? There are many misconceptions and confusion about the unconscious state known as coma. In this article, you will learn about the physiological processes that cause coma, how different a coma is in real life from the coma shown on television, and how often people wake up after being in a coma for months or even years.
What exactly is a coma?
The word coma comes from the Greek word koma. which means "sleep state". But being in a coma is not the same as sleeping. You can wake up those who are sleeping by talking to them or touching them. The same cannot be said about a comatose person - he lives and breathes, but unconsciously. He cannot respond to any stimuli (such as pain or the sound of a voice) or perform any independent actions. The brain still functions, but at the most basic level. To understand this, we must first look at the parts of the brain and how they work.
The brain is made up of three main parts: the cerebrum, the cerebellum, and the brainstem. The cerebrum is the largest part of the brain. It makes up the majority of the brain. The cerebrum controls cognitive and sensory functions such as intelligence, memory, thinking and emotions. The cerebellum is at the back of the brain and controls balance and movement. The brain stem connects the two hemispheres of the brain to the spinal cord. It controls breathing, blood pressure, sleep cycles, consciousness and other body functions. In addition, there are large masses of neurons under the brain called the thalamus. This small but very important area acts as a “relay” for sensory impulses in the cerebral cortex. For a more detailed explanation of brain function, look at how your brain works.
Scientists believe that consciousness depends on the constant transmission of chemical signals from the brain stem and thalamus of the brain. These areas, connected by neural pathways, are called the reticular activating system (RAS). Any interruptions in these signals can lead to an altered state of consciousness.
A vegetative state is a type of coma that presents a conscious but unconscious state of consciousness. Many of the patients who are in a vegetative state have previously been in a coma and after a few days or weeks they develop an unconscious state in which their eyelids are open, giving the impression that they are awake. Patients in this state of consciousness may behave in such a way that their family members incorrectly believe that they are finally out of the coma and communicative. Such actions may include grunting, yawning, and moving the head and limbs. However, these patients do not actually respond to any internal or external stimulation, indicating that extensive brain damage still persists. The outcome of patients whose vegetative state lasts for a month or more is usually poor and doctors use the term persistent vegetative state.
Other states of consciousness
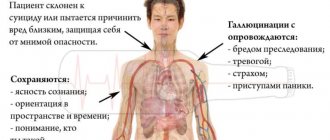
- Catatonia - People in this state do not move, do not speak, and generally do not make eye contact with other people. This may be a sign of mental disorders such as schizophrenia.
- Stupor —The patient can only be aroused by vigorous stimuli accompanied by physical activity that is free of uncomfortable or aggravating stimuli.
- Drowsiness - represents light sleep characterized by mild arousal and periods of activity.
- Communicating with the Eyes - People with this rare neurological condition have full ability to think and reason, but are completely paralyzed except for opening and closing their eyes (which they sometimes use to communicate). Strokes or other causes that cause damage to the brain stem, but not the brain itself, can lead to this syndrome.
- Brain death - People with this disease show no signs of brain function. Although their heart is still beating, they cannot think, move, breathe, or perform any bodily function. A person who is “brain dead” cannot respond to painful stimuli, breathe unaided, or digest food. Legally, the patient is declared dead and organ donation can be considered according to the wishes of the patient or his family.
How do people fall into a coma?
Medically induced coma
When the body is injured, it repairs itself through several mechanisms, including inflammation, which can cut off oxygen and blood flow to the brain. By putting a patient into a coma, doctors essentially put the brain into hibernation, reducing the amount of blood flow and oxygen the brain uses. This helps protect against tissue damage while the patient's body has a chance to recover.
In the fall of 2004, doctors in Wisconsin induced a seven-day coma in a 15-year-old girl with rabies, a disease that devastates the brain and often leads to death. After emerging from the coma, the girl began to recover.
Diseases that affect the brain and traumatic brain injuries can cause coma. If a person has suffered a severe head injury, the injury can cause the brain to move back and forth inside the skull. Movement of the brain inside the skull can tear off blood vessels and nerve fibers, causing the brain to swell. This tumor presses on the blood vessels, blocking the flow of blood (and with it, oxygen) to the brain. Parts of the brain that are deprived of oxygen and starved begin to die. Some infections of the brain and spinal cord (such as encephalitis or meningitis) can also cause swelling of the brain. Conditions that cause excess blood inside the brain or skull, such as a fractured skull or ruptured aneurysm (hemorrhagic stroke), can also lead to swelling and further damage to the brain.
A type of stroke called ischemic stroke can also lead to coma. This stroke occurs when the artery that supplies blood to the brain is blocked. When the brain is blocked, it lacks blood and oxygen. If it is very large, the person may fall into a stupor or coma.
In people with diabetes, the body does not produce enough of the hormone insulin. Because insulin helps cells use glucose for energy, a lack of the hormone causes blood glucose levels to rise (hyperglycemia). Conversely, when insulin is in the wrong proportion, in excess, blood sugar levels can drop too low (hypoglycemia). If blood sugar levels are either very high or too low, it can cause a person to fall into a diabetic coma .
Coma can also be caused by brain tumors, alcohol or drug overdose, seizure disorders, lack of oxygen to the brain (such as from drowning), or very high blood pressure.
A person may fall into a coma immediately or gradually. If an infection or other illness causes a coma, for example, a person may develop a high fever, become dizzy, or appear lethargic before falling into a coma. If the cause is a stroke or severe head injury, people may fall into a coma almost immediately.
How can you tell if someone is in a coma?
Coma can look different depending on the situation. Some people may lie completely still and not respond. Others will twitch or move involuntarily. If the respiratory muscles are damaged, the person will not be able to breathe on their own.
Doctors in the United States evaluate potentially comatose patients based on one of two scales: the Glasgow Coma Scale and the Rancho Los Amigos Scale. determining the degree of mental impairment by assigning a score from three to 15, with the third degree being the deepest coma, and at 15th they are usually taken out and taken out. The scale points are based on three main parameters:
The Rancho Los Amigos scale, developed by doctors at Rancho Los Amigos Hospital in California, helps doctors monitor the dynamics of recovery after a coma of a person who has suffered a head injury. This is most helpful during the first weeks or months after the injury.
Based on the results of these two scales, doctors diagnose patients with one of four states of consciousness.
- Comatose and unresponsive —the patient is unable to move or respond to stimuli.
- Comatose but responsive —the patient is unresponsive to stimuli, but there are reactions such as movement or rapid heart rate.
- Conscious but unresponsive —the patient can see, hear, touch, and taste, but cannot respond.
- Conscious and Responsive - The patient is out of coma and can respond to commands.
"Soap Opera Coma"
In soap operas, characters often fall into a coma after a car accident. The injured actress lies on a hospital bed (her makeup remains in excellent condition, of course). Doctors and family members are constantly at her bedside, urging her to live. In a few days, her eyes will be wide open and she will greet her family and doctors as if nothing had happened.
Unfortunately, a “soap opera coma” has little in common with a real-life coma. When a team of researchers studied nine television soap operas aired over a 10-year period, they found that 89 percent of soap opera characters made full recoveries. Only 3 percent of the heroes remained in a vegetative state, and 8 percent died (two of these heroes "came back to life"). In fact, coma survival is 50 percent or less, and less than 10 percent of people who come out of a coma make a full recovery from it. Although soap operas are not far removed from reality in many other ways, the study's authors were concerned that a "soap opera coma" might lead to unrealistic expectations among loved ones of people who are comatose in real life.
How do doctors “treat” patients in a coma?
There is no treatment that can bring you out of a coma. However, treatment can prevent further physical and neurological damage.
First, doctors ensure that the patient is not in immediate danger of dying. This may require placing a tube into the patient's windpipe through the mouth, and connecting the patient to a breathing machine, or ventilator. If there are other serious or life-threatening injuries to the rest of the body, they will be considered in descending order of importance. If excess pressure in the brain has caused a coma, doctors can surgically reduce it by placing tubes inside the skull and draining the fluid. A procedure called hyperventilation, which increases your breathing rate to compress blood vessels in the brain, can also relieve pressure. The doctor may also give the patient medications to prevent seizures. If a person in a coma is diagnosed with a drug overdose or a condition such as very low blood sugar that is responsible for the coma, doctors try to correct it as quickly as possible. Patients with acute ischemic stroke may undergo procedures or receive special medicine to try to restore blood flow to the brain.
silastroy.com The consumption of cement for the construction of brick walls should be carried out in advance. You can find out what the average cement consumption for bricklaying is from experienced specialists.
Doctors can use imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) to look inside the brain and look for tumors, pressure, and any signs of damage to brain tissue. Electroencephalography (EEG) is a test used to detect any abnormality in the electrical activity of the brain. It can also show brain tumors, infections and other causes that may cause coma. If a doctor suspects an infection such as meningitis, they might perform a spinal tap to make a diagnosis. To perform this test, the doctor inserts a needle into the patient's spine and removes a sample of cerebrospinal fluid for testing.
Once a patient's condition has been stabilized, doctors will concentrate on keeping him or her as healthy as possible. Patients who fall into a coma are susceptible to pneumonia and other infections. Many patients who fall into a coma remain in the hospital's intensive care unit (ICU), where doctors and nurses can constantly monitor them. People who are in a coma for a long time may receive physical therapy to prevent long-term muscle damage. Nurses also move them periodically to prevent bedsores, painful skin sores caused by lying in one position for too long.
Because comatose patients cannot eat or drink on their own, they receive nutrients and fluids through a tube into a vein or by bottle feeding so that they do not starve or become dehydrated. Coma patients may also receive electrolytes, which are salts and other substances that help regulate body processes.
If a patient is in a coma and depends on a ventilator to breathe for a long time, they may have a special tube inserted that goes directly into the windpipe through the front of the throat (tracheotomy). A tube inserted through the front of the throat can remain in place for a long period of time because it requires less maintenance and does not damage the soft tissue of the mouth and upper throat. Because a comatose patient cannot urinate on his own, a rubber tube called a catheter will be inserted directly into the bladder to remove urine.
Difficult decision
Caring for a spouse or family member in a coma or vegetative state is difficult enough, but when the condition persists for a long time, the family may have to make some very difficult decisions. In cases where a person cannot awaken from a coma quickly enough, the family must decide whether to keep their loved one on a ventilator and feeding tube indefinitely. Or stop supporting his life and allow the person to die.
If the person in question has written a will that includes medical directives, this decision is much easier to make because family members can simply follow the wishes of the comatose person. In the absence of a will, the family must consult carefully with physicians to determine what is best for the patient.
In a number of cases, the decision was controversial enough to end up in court—and in the headlines. In 1975, 21-year-old Karen Ann Quinlan suffered severe brain damage and fell into a permanent vegetative state after taking a dangerous mixture of sedatives and alcohol. Her family went to court to have Karen's feeding tube and the machine that helps her breathe removed. In 1976, a court in New Jersey agreed. However, Karen began breathing on her own after doctors removed her respirator. She lived until 1985, when she died of pneumonia.
A later case spawned even bigger battles in court, which reached the main office of the executors. In 1990, Terri Schiavo's heart temporarily stopped beating due to complications from bulimia. She suffered severe brain damage and fell into a permanent vegetative state. Her husband and parents asked the court to determine whether her feeding tube could be removed. Their dispute made its way into Congress, and even attracted the attention of President George W. Bush. Eventually the feeding tube was removed. Terri died in March 2005.
How do people “come out” of a coma?
How quickly a person recovers from a coma depends on what caused it and the severity of the brain damage. If the cause was a metabolic problem such as diabetes, and doctors treated it with medications, then the person may come out of the coma relatively quickly. Many patients who fall into a coma from a drug or alcohol overdose can also recover once their circulatory system is cleared of the substance that caused the coma. Coma caused by massive brain injury or a brain tumor may be more difficult to treat and may result in a much longer or permanent coma.
Most comas last between two and four weeks. Recovery is usually gradual, with patients showing more and more signs of "waking up" as time goes on. They may be "awake" and show it for only a few minutes on the first day, but gradually stay awake longer and longer. Research shows that a patient's recovery from a comatose state is very closely related to his or her degree of coma on the Glasgow Coma Scale. Most people (87 percent) who enter a stage three or four coma within the first 24 hours are likely to die or remain in a vegetative state. At the other end of the scale, about 87 percent of those in a coma are graded between 11 and 15 on the scale. The likelihood of them emerging from a coma is very high.
Some people emerge from a coma without any mental or physical disabilities, but most require at least some treatment to regain mental and physical skills. They may have to relearn how to talk, walk, and even eat. Others may never fully recover. They may regain some functions (such as breathing and digestion) and enter a vegetative state, but will never respond to stimuli.
Amazing awakenings
The story of Patricia White Bull is just one of many amazing stories of “awakening” from a coma. In April 2005, Donald Herbert "awakened" in a surprising way. A firefighter was seriously injured in 1995 when the roof of a burning building collapsed on him. He remained in a coma for ten years. However, when doctors gave him drugs commonly used to treat Parkinson's disease, depression and attention deficit disorder, Donald woke up and spoke to his family for a long 14 hours. Unfortunately, he died a few months later from pneumonia.
Not only are there amazing stories of “awakening” from comas, doctors have documented several cases of patients with severe brain damage suddenly regaining consciousness and talking to their family and friends. However, these are quite rare cases. In most cases, patients either “awaken” within days or weeks of entering a coma, or remain in a coma or vegetative state for the rest of their lives.
Symptoms and severity of coma
The comatose state, depending on the type and stage of the lesion, progresses and manifests itself with different symptoms. At the same time, there are signs of coma during a stroke, which make it possible to determine it against the background of fainting and clinical death of the patient. These include:
- a long period of the patient being unconscious - 2–3 hours or longer;
- low brain performance;
- weak and rare breathing;
- weak, practically unpalpable pulse;
- anisocoria or lack of response to light stimuli in both pupils;
- weak and slow heart rate;
- disturbance of heat exchange in the body;
- involuntary release of bowel movements;
- minimal response to all external stimuli or its complete absence.
Depending on the severity of the coma, symptoms may differ and intensify, which makes it possible to determine the prognosis of the patient’s further condition and development of events. There are 4 stages of coma in total:
- In the 1st degree, the patient stops responding to all kinds of stimuli or reacts inhibited, but he is still able to contact people, is able to swallow something, and also perform simple movements and roll over. This course of coma has a favorable prognosis.
- In the 2nd degree, the patient’s condition becomes semi-conscious, there is practically no response to stimuli, the breathing rhythm is lost, but the main reflexes are still present. The patient can survive only with a stable, non-progressive course of coma and proper care for him.
- At the 3rd, atonic degree, a person plunges into an unconscious state, he is completely unable to react in any way to all sorts of stimuli, and there are also no basic reflexes. The patient's muscle tone decreases significantly, convulsions occur, and blood pressure and body temperature rapidly drop. In this situation, the chances of survival are minimal.
- With the 4th degree of coma, the patient experiences areflexia and muscle atony. The pupils dilate, the temperature becomes critically low, breathing becomes weak and rare. With this course of coma, death occurs in a short time, and it is impossible to resuscitate the patient.
REFERENCE!
A comatose state manifests itself differently and individually in all people; often it may not progress to more severe stages, which increases the chances of a positive prognosis and further recovery of the patient.
It is impossible to determine exactly how many days or months a coma may last during a major stroke; it completely depends on the condition of the patient’s body and the characteristics of his care by doctors and relatives. On average, the period of coma lasts 2–14 days, but some severe cases can last for months or years.
It is important that treatment measures are taken on time, and then it will be possible not only for a person to quickly emerge from a coma, but also for his rehabilitation, since the level of possible future brain functionality depends on the duration and rate of progression of the comatose unconscious state.
Symptoms of change in condition
Symptoms are determined by the degree of inhibition of higher nervous activity. Depending on the depth, there are several types of this severe stroke complication.
| Types of stroke complications | Description |
| Prekoma |
|
| First degree |
|
| Second degree |
|
| Third degree |
|
| Extreme coma (4 degrees) |
|
What types of stroke are most likely to cause coma?
A person most often enters a comatose state during the development of a hemorrhagic form of stroke. This phenomenon occurs due to rupture of the walls of cerebral vessels due to a rapid increase in blood pressure, which leads to further hemorrhage in the brain. Under the influence of a large volume of blood, the areas affected by the stroke are compressed and gradually die. Such a pathological process in the body activates its defensive reaction, during which the person plunges into an unconscious comatose state. External factors also increase the risk of comatose loss of consciousness, including:
- hypertensive crisis;
- overheating of the body;
- severe injury;
- excessive and constant physical activity;
- constant stress state of the body.
ATTENTION!
Often, in the absence of positive dynamics within 2 days after the onset of coma, a person with a hemorrhagic stroke experiences death.
In more rare cases, coma occurs with an ischemic stroke, when there is no bleeding in the brain, but the organ is not saturated with oxygen. Such oxygen starvation provokes extensive damage to brain cells. In most of these cases, with the help of resuscitation methods, there is a chance to return the patient to consciousness, and the likelihood of recovery is quite high. Hemorrhagic stroke poses a great danger because it is easier to prevent than to cure; with this pathology there is a high risk of death for the patient.
A patient who has survived a coma with an ischemic stroke can subsequently live for many years and return to normal activities immediately after rehabilitation. Brain cells in this comatose state do not die, which is why the risk of complications and disability is much lower than with a hemorrhagic stroke.
The rarest cases are coma during a brainstem stroke, when the body plunges into a deep unconscious state gradually and slowly, with obvious symptoms of a stroke. Qualified medical staff can prevent the onset of coma, and if it does occur, they can quickly bring the patient out of it without further consequences.
REFERENCE!
A patient with a stroke in any form must be under constant supervision of medical personnel and undergo regular examinations (CT, MRI). Such methods can prevent the onset of coma and save a person.
Prognosis after ischemic, hemorrhagic
Cerebral hemorrhage usually occurs in a more severe form. The mortality rate in such patients reaches 70%; even after removal of the hematoma, the rate is not much lower. Unfavorable factors include:
- breakthrough of blood into the ventricles of the brain;
- uncontrolled arterial hypertension;
- large volume of hematoma;
- progressive cerebral edema;
- signs of displacement of the stem part;
- acute heart failure;
- increase in creatinine content in the blood;
- convulsive syndrome, lack of consciousness, reactions to painful stimuli for more than 3 days;
- age after 70 years.
With ischemic stroke, a more benign course is observed; it is rarely accompanied by a profound impairment of consciousness. This happens with repeated vascular accidents, massive blockage of the brain arteries with cholesterol plaques, lack of treatment or complete disregard of doctors’ recommendations.
gure>
Precoma and the first degree of coma can still give the patient a chance for recovery; with a higher degree, the prognosis is considered doubtful, and the onset of extreme coma is usually regarded as fatal.
When and why is a patient put into an artificial coma?
During a stroke, a critically serious condition of the patient may arise, when a drug-induced artificial temporary shutdown of his consciousness is required to prevent pathological irreversible changes in the brain that are life-threatening. This radical method is often used after a TBI with severe hemorrhages. Such cases require putting the patient into an artificial coma.
Long-term analgesia promotes vasoconstriction and a decrease in the intensity of cerebral blood flow, which avoids the death of brain tissue. An artificial coma can continue for as long as necessary to completely exclude necrosis. At this time, the patient must be under the control of doctors who conduct monitoring and the necessary studies and, based on their results, decide when to bring the patient out of the coma, also using medication.
Although an induced coma can prevent a person’s death, it leaves behind the following consequences:
- The occurrence of blood stagnation due to difficulties in the functioning of the cardiovascular system.
- Disorders of the nervous system due to disruptions in brain functionality during the recovery of the patient from a coma.
- Tracheobronchitis and pneumonia due to the use of a ventilator due to lack of oxygen during the progression of the stroke.
IMPORTANT!
Induced coma is a last resort method of treatment and is used extremely rarely when the risk of negative consequences is lower than the effectiveness of the procedure.
Pathogenesis of coma
Ischemic stroke most often ends in metabolic coma. Oxygen starvation forces the brain to switch to aerobic energy, which it receives by breaking down fatty acids. Literally five minutes of this process lead to acidification of the membranes of nerve cells with products of anaerobic glycolysis.
The cytoplasm enters the intercellular fluid and significantly increases its volume, and this is another compression of the capillaries and a secondary disruption of the blood supply to neurons. Ischemia occurs, cells switch to oxygen-free energy production and die by destruction.
Important! This process is avalanche-like and rapid, the more cells die, the greater the swelling, and the less chance other cells have to survive. In this case, a deep coma is most likely, because all the conditions have been created for it.
Hemorrhagic cerebral stroke is compression of the limbic areas of the brain or its cortex by a hematoma. Otherwise, the pathogenesis does not differ from that described above. And coma with a stroke of this type is also not uncommon.
Caring for a comatose patient
In order for the patient to come out of a coma as quickly as possible, he requires special care, which should be provided by medical facility staff and close relatives. The main components of proper care are:
- Nutrition. The supply of food is necessary to maintain the life of the patient. Products in powder form, resembling formula milk, must be introduced into the body using a tube.
- Vitamin droppers. The patient needs a mandatory supply of vitamins so that the body can strengthen its resistance to pathological changes.
- Hygiene. The patient's body should be wiped daily with a damp, soapy cloth. It is also necessary to clean his mouth and wash his hair at least once a week. You can use both regular hygiene products and special ones for caring for bedridden patients.
- Massage. To prevent the appearance of bedsores, the patient should regularly massage the areas of the shoulder blades, legs and buttocks. It is also recommended to purchase a special anti-decubitus mattress for it and periodically change its position.
- Medical equipment. Pressure and pulse sensors must be connected to the patient, and, if necessary, an artificial respiration apparatus. This equipment is needed to monitor a person’s condition.
IMPORTANT!
In severe cases of a coma with the development of an intracerebral hematoma, surgery is necessary to speed up recovery from the coma and increase the chances of a quick rehabilitation of the person.
Recognizing danger
Is it possible to come out of a coma? The sooner the danger is identified and appropriate measures are taken, the better the prognosis for the patient. How long does a coma last? Everything is individual here. This could be a couple of hours, or maybe several days.
It is extremely rare that this period is calculated in months. It is possible that the stroke will last for years, but in this case, relatives should not reassure themselves of a favorable outcome.
Signs accompanying coma from a stroke are as follows:
- speech becomes quiet and incoherent;
- the patient may be in a state of delirium and confusion;
- the body becomes sluggish;
- gagging occurs;
- breathing quickens;
- there is no reaction to any stimuli.
It is the last sign that is coma in both hemorrhagic and ischemic strokes.
Treatment and recovery from coma
To recover from a coma after a stroke, treatment is necessary, depending on the form of the disease. So, in case of hemorrhagic stroke, it is necessary to perform surgery to remove the hematoma in the brain area. Then the patient should be connected to a ventilator and equipment that monitors the body’s indicators and supports its vital functions.
If the comatose state occurs as a result of an ischemic stroke, it is necessary to treat the patient with the use of anticoagulants (Heparin, Aspirin) and drugs that stimulate the blood supply to the central nervous system (Actovegina, Nooholina).
In addition, regardless of the type of stroke suffered, the patient needs antibiotics (Levomycetin and analogues) and hepatoprotectors to protect the liver from active drugs (Phosphogliv, Rezalut).
After emerging from a comatose state, long-term rehabilitation of the patient is necessary, which takes place in stages:
- First, basic reflexes (in particular swallowing) and the ability to respond to external stimuli are restored. The patient can also turn his head.
- Consciousness slowly but gradually returns, however, hallucinations of various types are present, which indicates positive dynamics and recovery of the patient. During the same period, memory, visual and speaking functions partially return.
- The patient begins to move smoothly, the ability to sit and stand up returns.
IMPORTANT!
The stages of rehabilitation require great physical and moral costs not only for the patient, but also for his relatives, since they must help him recover. Relatives should make every effort to prevent the progression of the stroke and its recurrence.
Relatives of a person who has emerged from a coma should create exceptionally favorable conditions for rehabilitation. They need:
- praise the patient for every small progress;
- create a positive attitude for the patient, reassure him;
- avoid conflicts and difficult psychological situations;
- learn how to massage to restore body functions in a patient;
- pay as much attention as possible to the patient;
- engage in special physical exercises with the patient.
Relatives must remember: the longer a person has been in a comatose state, the more time and effort his rehabilitation will take. It is important not to let him despair and promote recovery by actively working with him.
Treatment
In the event of a stroke with hemorrhage, a hematoma in the brain is surgically removed, which increases the chances of recovery.
Ischemic stroke and who is treated as a result of it in neurological intensive care. If significant functions are impaired, the patient is connected to a ventilator, and the main indicators are displayed on the monitor. Euthanasia is prohibited in the Russian Federation, therefore, given how many days the coma lasts, that is how long it is necessary to maintain life with the help of medical equipment, food, and care.
Anticoagulants and nootropics are prescribed for the treatment of ischemic stroke. The first group includes Warfarin, Aspirin and other medications with similar effects. This prevents blood thickening and thrombosis and facilitates blood circulation through the vessels. Including the brain. The second group includes: Actovegin, Cavinton, Cerebrolysin and other medications that improve brain activity, help normalize the functioning of the central nervous system, etc.
Source: telemedicina.one
Prevention
After a stroke, a coma often occurs, especially if the person is older, but he tries to ignore all the signs of what is happening.
After regaining consciousness, the patient can talk about the following moments:
- impaired speech abilities;
- manifestation of yawning;
- active dizziness;
- increased breathing;
- pale skin;
- paresthesia with elements of numbness or manifestations in certain parts of the body.
In order to avoid this condition, it is necessary to take measures aimed at preventing the occurrence of a stroke.
It is important to take full responsibility for your condition and lead a healthy lifestyle in order to avoid the occurrence of pathological processes in brain cells. It is also worth studying the symptoms of an attack and, at the slightest occurrence, rush to seek the help of specialists
It is also worth studying the symptoms of an attack and, at the slightest occurrence, rush to seek the help of specialists.
What to expect?
How positive the prognosis will be depends on many factors. Do not forget that coma and stroke are in themselves severe phenomena for the body. Therefore, you should not expect a completely favorable outcome.
Most often, this is a fatal outcome, or a situation where the patient’s condition does not improve for a long time, and it all ends with either euthanasia or death. Despite the sad statistics, there is a chance that a patient after a stroke can not only survive, but also fully or partially restore lost functions. And this is influenced by:
- the location where the stroke lesion occurred;
- how extensive it was;
- how long the patient was without medical care;
- what stage of coma does the patient have;
- duration of stay in a comatose state.
The age of the patient is also important; most often, favorable prognoses are given to younger people. And the older the patient is, the less likely he is to emerge from a coma with minimal consequences, especially if the stroke was of a hemorrhagic type.
Even if the patient was able to restore the functions lost during the coma and return to social life, neuralgic complications will remain with him, and he will need to constantly monitor his condition to exclude the possibility of a relapse.
What does this condition lead to?
The consequences of a stroke with coma are as follows:
- people recover completely, retaining all the functions that were lost during the coma. An atrophic cyst forms at the site of hemorrhage;
- Those who recover from a coma cannot restore the functions lost in a coma after a stroke. A person can only partially recover, so plegia, paralysis and confusion do not leave him for a long time;
- a vegetative state when the patient comes out of an extremely deep coma. The length of stay in it depends not only on the patient’s condition, but also on the maintenance of blood pressure by dopamine. Usually this takes a day, no more;
- impaired respiratory function and/or malfunction of the cardiac system leads to agony, in which the prognosis is the worst - death.