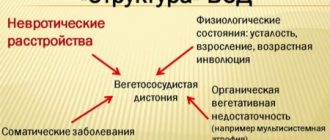
VSD can hardly be called a disease; rather, it is a collection of symptoms. Science classifies this condition as a pathological phenomenon occurring in the central nervous system. The International Classification of Diseases (abbreviated as ICD) does not contain VSD; this condition occupies a range from G00 to G99. However, dystonia cannot be found here either; it is only mentioned in category G90.8 - under the title “Other disorders of the nervous system.”
Basic VSD codes in the ICD
The diagnosis of “vegetative-vascular dystonia” is made only in our country - ICD-10 does not distinguish VSD as a separate disease. Therefore, the alphanumeric designation of the disease is selected based on the prevailing symptoms of VSD and disorders identified during diagnosis.
Vegetative-vascular dystonia is designated by a code in the range G00-G99. These numbers indicate pathologies of the nervous system. For example, a disease can be encrypted:
- G99.0* - autonomic neuropathy with endocrine and metabolic disorders;
- G99.1* - includes other disorders of the autonomic nervous system occurring against the background of concomitant diseases;
- G99.8* - denotes specified disorders of the nervous system in diseases classified in other headings.
VSD according to ICD-10 may have the code R45, which indicates symptoms related to the emotional sphere of a person.
- Diagnosis is often coded under R45.8, which stands for Other Symptoms and Signs Relating to Emotional State.
- Code F45.3 is used primarily by neuropsychiatrists. Alphanumeric coding determines changes in well-being in adult patients with a symptom complex of disorders characteristic of somatoform dysfunction of the ANS.
When assigning a disease code, the type of VSD is also taken into account - hypertensive, hypotensive or mixed nature of the syndrome.
Vegetative-vascular dystonia in children :: Symptoms, causes, treatment and code according to ICD-10
Title: Vegetative-vascular dystonia in children.
Vegetative-vascular dystonia in children
Vegeto.
Vascular dystonia in children is a symptom complex of functional disorders of various systems caused by a violation of the regulation of their activities by the autonomic nervous system.
Vegetative-vascular dystonia in children can manifest itself as cardiac, respiratory, neurotic syndromes, vegetative-vascular crises, and thermoregulation disorder syndrome.
Diagnosis of vegetative-vascular dystonia in children includes a functional examination of the cardiovascular, nervous, and endocrine systems (ECG, EEG, EchoCG, EchoEG, REG, rheovasography, etc.). In the treatment of vegetative-vascular dystonia in children, medication, physiotherapy, and psychological effects are used.
Vegetative-vascular dystonia in children is a secondary syndrome that affects various somato-visceral systems and develops against the background of deviations in the autonomic regulation of the functional state of the body. According to various data, certain signs of vegetative-vascular dystonia are diagnosed in 25-80% of children.
More often, the syndrome is found in children 6-8 years old and in adolescents, predominantly female.
In pediatrics, vegetative-vascular dystonia is not considered as an independent nosological form, therefore, various narrow disciplines are studying its manifestations: pediatric neurology, pediatric cardiology, pediatric endocrinology, pediatric gastroenterology, etc. Autonomic disorders in children can give impetus to the development of serious pathological conditions - arterial hypertension, bronchial asthma, gastric ulcer, etc. On the other hand, somatic and infectious diseases can aggravate vegetative changes.
Vegetative-vascular dystonia in children The causes of the formation of vegetative-vascular dystonia in children are often hereditary in nature and are caused by deviations in the structure and functioning of various parts of the autonomic nervous system on the maternal side. The development of vegetative-vascular dystonia in a child is facilitated by the complicated course of gestation and childbirth: toxicosis of the pregnant woman, fetal hypoxia, intrauterine infections, rapid or prolonged labor, birth injuries, encephalopathy, etc. A special role in the development of vegetative-vascular dystonia in children belongs to various psychotraumatic influences - conflicts in the family and school, pedagogical neglect of the child, overprotection, chronic or acute stress, increased school loads. Predisposing factors for vegetative-vascular dystonia in children can be somatic, infectious, endocrine diseases, neuroinfections, allergies, focal infections (chronic tonsillitis, caries, pharyngitis, sinusitis), constitutional abnormalities, anemia, traumatic brain injuries. The direct triggers of autonomic dysfunction in most cases are unfavorable weather conditions, climatic features, unfavorable environmental conditions, physical inactivity, imbalance of microelements, excessive physical activity, poor nutrition, violation of the daily routine, insufficient sleep, hormonal changes during the puberty period. Manifestations of vegetative-vascular dystonia in children manifest themselves during periods of active growth of the child, when the functional load on the body is especially high and the nervous system is labile.
Autonomic disorders are accompanied by various reactions of the sympathetic and parasympathetic systems, caused by impaired production of corticosteroids, mediators (acetylcholine, norepinephrine), biologically active substances (prostaglandins, polypeptides, etc.), impaired sensitivity of vascular receptors.
When diagnosing vegetative-vascular dystonia in children, a number of criteria are taken into account, which are decisive in distinguishing the forms of the syndrome. According to the predominant etiological signs, vegetative-vascular dystonia in children can be psychogenic (neurotic), infectious-toxic, dyshormonal, essential (constitutional-hereditary), mixed in nature. Depending on the nature of autonomic disorders, sympathicotonic, vagotonic and mixed variants of vegetative-vascular dystonia in children are distinguished. Taking into account the prevalence of vegetative reactions, vegetative-vascular dystonia in children can be generalized, systemic or local.
According to the syndromological approach during vegetative-vascular dystonia in children, they distinguish between cardiac, respiratory, neurotic syndromes, thermoregulation disorder syndrome, vegetative-vascular crises, etc. According to the severity, vegetative-vascular dystonia in children can be mild, moderate and severe; according to the type of flow - latent, permanent and paroxysmal.
The clinical picture of vegetative-vascular dystonia in a child is largely determined by the direction of autonomic disorders - the predominance of vagotonia or sympathicotonia. About 30 syndromes and more than 150 complaints accompanying the course of vegetative-vascular dystonia in children have been described. Cardiac syndrome of vegetative-vascular dystonia in children is characterized by the development of paroxysmal cardialgia, arrhythmia (sinus tachycardia, bradycardia, irregular extrasystole), arterial hypotension or hypertension. In the case of a predominance of cardiovascular disorders in the structure of vegetative-vascular dystonia, they speak of the presence of neurocirculatory dystonia in children. Neurotic syndrome with vegetative-vascular dystonia in children is the most constant. Typically, the child complains of fatigue, sleep disturbances, poor memory, dizziness, headaches, and vestibular disorders. Children with vegetative-vascular dystonia experience low mood, anxiety, suspiciousness, phobias, emotional lability, and sometimes hysterical reactions or depression. With leading respiratory syndrome, shortness of breath develops at rest and during physical stress, periodic deep sighs and a feeling of lack of air are noted. Violation of thermoregulation in vegetative-vascular dystonia in children is expressed in the occurrence of intermittent low-grade fever, chills, chilliness, poor tolerance of cold, stuffiness and heat. Reactions of the digestive system can be characterized by nausea, increased or decreased appetite, unmotivated abdominal pain, and spastic constipation. The urinary system is characterized by a tendency to fluid retention, swelling under the eyes, and frequent urination. Children with vegetative-vascular dystonia often have marbled coloration and increased greasiness of the skin, red dermographism, and sweating.
Constipation. Lack of air. Dyspnea. Chills. Sweating. Nausea. Emotional lability.
Children with vegetative-vascular dystonia need consultation with a pediatrician, as well as (in accordance with the leading causes and manifestations) a pediatric neurologist, pediatric cardiologist, pediatric endocrinologist, pediatric gastroenterologist, pediatric otolaryngologist, and pediatric ophthalmologist. The initial autonomic tone and autonomic reactivity are assessed using the analysis of subjective complaints and objective indicators - ECG data, Holter monitoring, orthostatic, pharmacological tests, etc. To assess the functional state of the central nervous system in children with vegetative-vascular dystonia, EEG, REG, EchoEG, and rheovasography are performed.
During the diagnosis, other pathologies that have similar clinical manifestations are excluded: rheumatism, infective endocarditis, juvenile arterial hypertension, bronchial asthma, mental disorders, etc.
When choosing methods for treating vegetative-vascular dystonia in children, the etiology and nature of autonomic disorders are taken into account. Preference is given to non-drug therapy. General recommendations include normalizing the daily routine, rest and sleep; dosed physical activity; limiting traumatic influences, consulting a family and child psychologist, etc.
For vegetative-vascular dystonia in children, courses of general massage and massage of the cervical-collar zone, IRT, physiotherapy (electrophoresis on the collar zone, endonasal electrophoresis, galvanization, electrosleep), exercise therapy have a positive effect.
Water procedures are useful: swimming, therapeutic showers (circular, fan, Charcot shower), general baths (turpentine, radon, pine, carbon dioxide). An important role in the complex therapy of vegetative-vascular dystonia in children is given to the treatment of focal infection, somatic, endocrine, etc. diseases.
If it is necessary to include drug therapy, sedatives, nootropics, multivitamin complexes are used, and, according to the indications of a pediatric psychoneurologist, antidepressants or tranquilizers are used.
Consistent prevention, timely diagnosis and treatment of autonomic disorders can significantly reduce or eliminate the manifestations of vegetative-vascular dystonia in children. In the case of a progressive course of the syndrome, children may subsequently develop various psychosomatic pathologies, causing psychological and physical maladaptation of the child.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: https://kiberis.ru/?p=32832
Codes for hypertensive form of dystonia
The hypertensive variant of VSD is characterized by a periodic increase in blood pressure. Hypertension manifests itself:
- discomfort;
- severe headaches;
- nausea;
- loss of strength.
The code is selected based on the development of hypertension:
- Code I10 indicates primary hypertension. The patient has not been diagnosed with organic pathologies that can cause pressure surges.
- Code I15 is used if hypertension in VSD is secondary and develops against the background of some pathology.
The main ICD-10 code may be supplemented by others depending on concomitant VSD diseases.
Codes for hypotensive form of dystonia
Hypotension in dystonia manifests itself:
- loss of strength;
- increased drowsiness;
- yawning;
- tachycardia;
- internal trembling.
During an acute attack of arterial hypotension, the following symptoms appear:
- darkening before the eyes;
- unsteadiness and uncertainty of gait;
- severe dizziness;
- fainting (in severe cases).
The hypotonic type of VSD is most often referred to as code F45.3, which denotes somatoform dysfunction of the autonomic nervous system. The disease is also encrypted with codes:
- I95.0 - idiopathic hypotension;
- I95.1 – orthostatic hypotension that occurs when standing up;
- I95.8 – other types of hypotension;
- I95.9 – hypotension of unspecified etiology.
To select the correct section in the international classification of diseases, the doctor carefully collects anamnesis, determines the mechanism of development of the disease and determines the influence of organic pathologies.
Neurocirculatory dystonia (NCD) is encrypted in the international classification of diseases with code F45.3. This designates somatoform dysfunctions that occur with episodes of heart rhythm disturbances and blood pressure instability.
Treatment of vegetative neuroses
VSD is not life-threatening, but it greatly complicates it, and in order to alleviate the patient’s condition, he is prescribed medications to regulate blood pressure, painkillers, antispasmodics, and sleeping pills. But the painful symptom complex resembles a bouquet of poisonous flowers that grow from the same root. To destroy them, you need to remove the root. And since, according to ICD 10, dystonia is based on neuropsychiatric disorders, it is necessary to fight not only its vascular and other manifestations, but also the cause.
If a medical examination shows that a person does not have organic disorders that could confirm his complaints, treatment is organized in such a way as to normalize his neuropsychic state. He is prescribed sedatives, a relaxing or tonic massage, physiotherapy, moderate physical activity, and is recommended to reconsider his lifestyle. In severe cases, you need the help of a psychologist or psychotherapist. Such treatment is always long-term and should not be interrupted prematurely.
But it must be borne in mind that since ICD 10 and other official documents do not consider vegetative neurosis a disease, there is no standard therapeutic regimen. For the same reason, there are no exact criteria for assessing the effectiveness of treatment, and we have to judge this only by how we feel.
How codes are set for children with VSD
Identification of disease codes according to the ICD in children is no different from encoding diagnoses in adult patients. The development of dystonia in a child may be associated with:
- somatic;
- infectious diseases.
In this case, VSD is a secondary pathology, so the alphanumeric designation of the primary disease is indicated first. Dystonia developing in a child is coded by a pediatric neurologist.
The International Classification of Diseases is a document approved by the World Health Organization. According to generally accepted regulations, certified doctors treating private and public medical institutions are required to use the specified disease encryption standards in their practice.
The use of ICD codes is important not only for studying the characteristics of pathologies and determining the frequency of their detection. Thanks to universal disease coding, patients do not have to worry about how they will communicate their diagnosis to doctors who do not speak their language.