Dementia is a decrease in a person’s intellectual abilities, in which memory, thinking, behavior in society and social adaptation are impaired.
If such changes are congenital or appear in the first years of a child’s life, we are talking about mental retardation. If intelligence decreases due to various diseases and injuries after three years of life, including in adults and old age, we talk about acquired dementia, that is, dementia.
According to statistics, intellectual disabilities occur in approximately every hundredth person on Earth, that is, this is a very common disorder. As we see, in order to understand what dementia is and to assess the severity of changes, you will first have to understand the meaning of some terms.
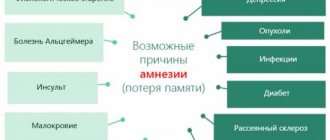
Causes of dementia
Dementia in adults, in which symptoms appear gradually, occurs for a number of reasons. The main one is the development of pathologies characterized by the death of brain cells.
These include:
- neurodegenerative diseases;
- pathologies of the central nervous system;
- neuronal atrophy;
- multiple sclerosis.
Senile dementia can occur as a complication after the following pathologies:
- inflammation of the spinal cord and brain;
- traumatic brain injuries (open and closed type);
- benign and malignant tumors;
- drug poisoning;
- alcohol addiction;
- high blood pressure;
- acute cerebral circulatory disorder;
- vascular atherosclerosis.
Risk factors contributing to the development of dementia include:
- lack of intellectual activity for a long time;
- obesity;
- diabetes;
- genetic predisposition (if there are relatives suffering from dementia).
Statistically, dementia occurs more often in women than in men.
Causes and risk factors
Interestingly, this disease is much more common among women than among men.
This can be explained by a different structure of the psyche: dementia against the background of schizophrenia develops with strong fears and stress, to which women are more susceptible than men.
In this case, cognitive abilities are not completely lost, but remain, as it were, in a “frozen” state.
In psychiatry, there are four risk groups that are at risk of schizophrenic dementia:
- People with an unstable nervous system. Schizophrenia in such cases manifests itself during a prolonged stay in a stressful state, as a result of which hallucinations may appear, but personality changes do not yet occur in the first stages of the development of the pathology. Such changes develop over time and are noticeable only to the patient’s closest relatives.
- Patients with a genetic predisposition to schizophrenia. Research shows that schizophrenia is transmitted through the female line, but children of both sexes can inherit the pathology. From a physiological point of view, this is explained by the fact that in people with such a predisposition, protein is synthesized faster in the body, which provokes metabolic disorders that affect the mental state.
- People with pathological changes in the brain affecting metabolic processes between neurotransmitters. As a result of such disorders, the transmission of nerve impulses becomes unstable, and any severe stress (even short-term) leads to schizophrenia with dementia developing against its background.
The fourth risk group includes exclusively young mothers who have recently given birth and still cannot get used to the sudden change in their social status. An additional provoking factor is constant lack of sleep and emotional turmoil associated with lifestyle changes in the first months of motherhood.
Currently, psychiatry, which is still considered a “young” science, cannot accurately describe all possible risk factors, therefore, in contrast to the more predictable senile dementia, the schizophrenic type of such a disorder cannot be predicted in advance in a particular person.
Classification of dementias
Dementia in adults (pathology symptoms are presented later in the article) is classified according to the following criteria:
- localization of the lesion;
- reason for development.
Based on location, the following types of dementia are distinguished:
- Multifocal. Almost the entire brain is affected. The patient has a violation of the mental processes responsible for the perception of information. The pathology progresses quickly.
- Cortical-subcortical. Mixed type dementia develops due to the destruction of the subcortical structures of the brain and its cortex.
- Cortical. The cause of this type of dementia can be considered Alzheimer's or Pick's disease. Characteristic symptoms include behavioral disturbances, memory loss and confusion.
Dementia can occur due to:
- Multiple sclerosis . The cause of development is the destruction of myelin sheaths. Patients complain of memory impairment and the inability to concentrate on anything.
- Epilepsy . Pathology cannot be called the root cause of dementia. The disease develops as a result of injuries received during a fall, after oxygen starvation and long-term use of phenobarbitals. The patient's emotional sphere is affected, the will is completely suppressed. Unmotivated aggression may occur.
- Injury _ Dementia is rare due to single injuries. Much depends on their repetition.
- Alcoholism . Systematic consumption of alcoholic beverages in large doses leads to disruption of the parts of the brain responsible for coordinating thinking, movement and memory. In the later stages of alcoholic insanity, the patient degrades.
- Pick's or Alzheimer's diseases . Pathologies are characterized by memory impairment: brain cells atrophy. With rapid progression, the patient is completely maladapted and disoriented.
- Vascular pathologies . A number of diseases accompanied by impaired blood circulation in the brain can trigger the development of vascular dementia. Characteristic symptoms include deterioration in thinking and memory, emotional disturbances and various mental disorders.
The exact causes of idiopathic dementia have not been identified. The characteristic symptom complex resembles the signs of Alzheimer's type dementia: cognitive functions are lost, the patient complains of movement and memory impairments.
Causes leading to mental weakness, classification
More than 200 pathological conditions lead to dementia.
According to their prevalence, the following are distinguished:
- Organic brain lesions. Among them, the leading place belongs to Alzheimer's disease. It causes about 50-60% of all cases of dementia.
- Vascular pathologies: atherosclerosis, hypertension. These diseases are detected in 20% of patients.
- Substance addiction, trauma, infection.
The reasons may be combined. The incidence rate is currently increasing.
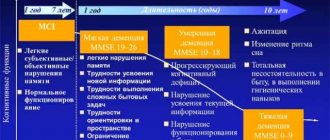
Severity of dementia
Dementia in adults, whose symptoms vary depending on the cause, can be classified by severity. Pathological manifestations arise gradually.
Based on the totality of cognitive impairment, the following degrees are distinguished:
- light;
- average;
- heavy.
The mild degree is characterized by the following manifestations:
- lack of interest in your favorite hobby;
- reluctance to communicate with others;
- development of depression, anxiety and tearfulness;
- the emergence of a critical attitude towards oneself;
- violation of the intellectual sphere and memory;
- partial preservation of the ability to self-care;
- limitation or partial loss of ability to work.
The patient's maladaptation is expressed in the refusal to take part in work and communication with loved ones. A person withdraws into himself, tries to spend more time alone and avoid visiting crowded places. The feeling of inferiority is provoked by a slowdown in the pace of thinking; patients complain of poor memory.
Signs of moderate dementia:
- pickiness;
- waywardness;
- vindictiveness;
- malice;
- aggressiveness.
The patient's depressive and anxiety states worsen. A manifestation of psychosis, accompanied by delusional ideas, is possible. The patient cannot think in detail; he is fixated on the same thought or situation for a long time. The patient ceases to orient himself in time and complains of a decrease in speech, auditory and visual memory.
The patient is unable to use household appliances and is unable to open and close the door lock. A person forgets how to use a mobile phone, but retains self-care skills.
With severe dementia, complete emotional impoverishment is observed. The patient's willpower is broken, he is unable to navigate in space. At this time, a person ceases to recognize himself as a person, cognitive activity is reduced. Fragmentary facts and events are retained in memory.
The thinking is viscous, the vocabulary is poor, the patient loses the ability to pronounce connected sentences. Self-care skills are lost, the person needs foster care.
Warning Sign #1: Problems with short-term memory.
We all forget where we put our keys sometimes, but if you find yourself forgetting something that happened recently more often, it could be a sign of dementia.
With short-term memory problems, a person may remember something that happened decades ago, but not what they did the day before.
Early symptoms of dementia
Dementia in adults (symptoms will be described in more detail later in the article) has no cure.
Symptoms of dementia in adults
With the help of drug therapy, the severity of characteristic symptoms can be reduced and the patient’s condition can be stabilized. The patient has difficulty communicating and begins to forget important dates.
Difficulty finding the right word
Difficulty finding suitable words is considered the earliest symptom of senile dementia. A person cannot clearly express his thoughts; pauses slip through the dialogue. The patient needs time to find the right word and continue the conversation.
Anxiety, suspiciousness
Suspiciousness and anxiety are considered a sign of dementia if a previously cheerful and open person began to be suspicious of close friends and relatives. The patient shows confidence, he is haunted by obsessive ideas and thoughts. It seems to a person that others are biased towards him.
Constant mood swings, depression
The process of destruction of brain cells is accompanied by the development of disorders of the endocrine system. In the human body, the production of hormones responsible for regulating mood is slowed down. In this case, the risk of depression is quite high.
Personality changes
Personality changes indicate the emergence of new character traits. A previously sociable, outgoing person becomes more shy, and a cheerful person turns into a grumpy and dissatisfied person. Personality defects are accompanied by a loss of values, attitudes and specific character traits.
Increased forgetfulness
Forgetfulness is another sign of dementia. An elderly person gradually begins to forget not only important dates, but also events that occurred more recently.
He does not remember the topics of the conversation, he is not able to remember what he ate for lunch or dinner. The patient may lose personal items, forgetting them on the street or in public places.
Disorders of orientation in time and space
An elderly person suffering from dementia ceases to navigate in space and time. The patient cannot remember the date of the celebration or the day of the week. Disorientation is often accompanied by a disturbance of consciousness: the patient ceases to recognize colleagues, friends and relatives.
Loss of interest in hobbies
Loss of interest in a hobby that previously brought pleasure and pleasure indicates the development of dementia in an elderly person. The symptom is stable, over time it becomes a personal feature: the patient ceases to experience positive emotions from life.
Loss of ability to follow conversational logic or verbosity
An elderly person suffering from dementia loses the ability to focus attention on the interlocutor. He is constantly distracted by what is happening around him, a conversation related to one or another event suddenly flows into another direction. A person cannot clearly formulate a thought and gets stuck in memories.
Tendency to constantly rearrange, hide, accumulate objects
With dementia, memory and personality deteriorate. An elderly person becomes suspicious and develops a need to collect. The patient begins to accumulate pieces of furniture and clothing, and hide personal belongings (including money) from relatives. People often forget where the cache is.
Aimlessness
With dementia, a person loses the ability to plan something and concentrate on one object. He can leave home to go to the store and return empty-handed.
The patient walks aimlessly around the house or street, asking the same questions, forgetting that he had already received answers to them.
How to help someone with dementia
Caring for the patient and his relatives, as well as their support, is the main cure for dementia. It is strictly forbidden to move such a person to a place that is unusual for him (no to sanatoriums and rest homes!), because of the change of environment, he will only get worse.
But how should relatives behave correctly so as not to injure the patient even more? There are some tips:
- your speech should be smooth and slow. There is no need to suddenly raise your tone, or even suddenly change your intonation. The fact is that weak-minded people may have difficulty distinguishing words, but they perfectly understand the intonation with which these words were spoken;
- check whether you managed to attract the patient’s attention to your words. As dementia progresses, it can become difficult to perceive whether a person understands you or not. To make sure whether you managed to reach him, you can carefully take his hand and look straight into his eyes. Also, it is advisable that you are at the same level - either both are sitting, or both are standing, etc.;
- start the conversation first. The patient may want to talk to you, but over time it will be difficult for him to start a conversation on his own. Take the time and effort to say a few phrases to the person. The time will come when there will be no one to look into the eyes and no one to talk to;
- formulate questions correctly. You must learn to ask questions that can be answered in one short word: yes, no, I don’t know. Thus, even if it is very difficult for the patient to tell you something, he will be able to at least clarify the situation a little;
- talk about the past. People with dementia are better able to remember things that happened years ago than what they had for breakfast this morning. Talk to patients about the past that they remember, this can calm them down a little.
Unfortunately, medications that could cure senile dementia have not yet been invented, however, there are drugs that will partially slow down the progression of dementia, improve sleep, and relieve increased irritability and dysphoria. And thanks to the above tips, you can make the patient’s life more comfortable and calm.
Main symptoms of dementia
Dementia in adults is an incurable disease that progresses due to injury, alcoholism or vascular pathologies. The main symptoms may vary depending on the type of disease.
Alzheimer's type dementia
The disease is characterized by damage to brain cells. Most often it occurs in old age. Patients experience a partial loss of intelligence; they stop remembering important events.
Cognitive functions are impaired, gradual degradation occurs. As Alzheimer's type dementia progresses, a person loses the ability to self-care.
The main symptoms of the pathology are:
- partial loss of vision;
- violation of spatial orientation;
- loss of ability to perform household tasks;
- aggressive behavior;
- absent-mindedness;
- forgetfulness;
- mood swings;
- memory impairment;
- detachment or depression.
A person feels uncomfortable even in his usual environment. As the disease progresses, the patient's condition will worsen.
Senile dementia with Lewy bodies
Dementia with Lewy bodies is characterized by autonomic, motor, mental and cognitive impairment. The disease is accompanied by neurodynamic disorders, which manifest themselves as a lack of ability to concentrate on anything.
Signs of DLB include:
- delirium;
- rave;
- dissociative disorder;
- psychomotor overexcitement;
- apathy;
- visual agnosia;
- amnesia;
- bradycardia;
- depression.
In the early stages, an increase in tone and a hypothetical syndrome are observed. Possible development of autonomic dysfunction.
Symptoms of vascular dementia
Dementia of the vascular type does not always lead to disturbances in the psychoemotional state.
Neurological symptoms may occur, which include:
- bulbar disorders;
- swallowing disorders;
- epileptic seizures;
- fatigue;
- increased anxiety;
- viscosity of thinking;
- verbosity;
- emotional lability.
The patient becomes more irritable and deliberately provokes conflict over trifles. Emotional generalized rigidity is observed in the final stage of vascular dementia.
Alcoholic dementia
Alcoholic dementia occurs due to prolonged abuse of alcoholic beverages. Ethyl alcohol damages brain cells by penetrating the blood-brain barrier. Alcohol-induced dementia most often occurs in people who have been dependent on alcohol for 10 years or more.
Typical symptoms include:
- constriction of the pupils;
- incoherence of words;
- sleep disorders;
- uncontrollable craving for collecting;
- lack of self-care skills;
- constant feeling of hunger;
- inability to concentrate on anything;
- spatial and temporal disorientation;
- depression;
- mood swings (from aggression to infantility);
- amnesia.
A person suffering from alcoholic dementia experiences periodic lucidity.
For a short period, the patient tries to return to a normal lifestyle: he recognizes loved ones, speech becomes coherent, and memory is restored. Periodic enlightenment occurs only in the early stages of alcohol addiction.
Epileptic dementia
This type of dementia occurs in people with epilepsy. Symptoms may vary depending on the stage of the disease. The main cause of development is considered to be cerebral hypoxia, which occurs during and after a seizure.
Symptoms of epileptic dementia include:
- unproductive, viscous speech;
- difficulty thinking;
- pathologically detailed speech;
- inability to express your thoughts;
- mood swings;
- anxiety;
- memory impairment;
- inhibited speech reactions.
At the early stage of epileptic dementia, a person is able to take care of himself. The patient requires care for moderate to severe forms.
Atrophic dementia
Atrophic dementia is a classic type characterized by the following symptoms:
- speech disorders;
- partial amnesia;
- verbosity;
- isolation;
- anxiety;
- physical degradation.
Personality breakdown is common in moderate to severe forms of dementia.
Mixed dementia
The following symptoms are typical for mixed type dementia:
- memory impairment;
- cognitive disorders;
- inability to concentrate;
- decreased productivity of intellectual work;
- spatial disorientation.
Patients suffering from mixed dementia have a history of atherosclerosis or stroke.
Terminal marantia dementia.
⇐ PreviousPage 18 of 24Next ⇒Terminal dementia (Bleicher V.M., 1976) is a manifestation of gross and massive destructive changes in the brain in severe debilitating diseases. It is characterized by a complete collapse of mental activity, leveling out the specificity of the previously existing dementia syndrome, and mental insanity.
V.M. Bleicher (1976) proposed a differentiated phenomenological taxonomy of dementia: 1) simple dementia, characterized by negative symptoms; 2) psychopathic-like dementia, in which, along with some intellectual-mnestic decline, a sharpening of negative premorbid personality traits or its new abnormal features manifests itself; 3) hallucinatory-paranoid dementia, in the structure of which hallucinations and delusions are closely linked with dementia; 4) amnestic-paramnestic dementia (with Korsakoff syndrome); 5) paralytic and pseudoparalytic dementia; 6) asemic dementia, characterized by the presence of signs of focal damage to the functions of speech, gnosis and praxis; 7) terminal dementia. The author emphasizes that, manifesting itself within the framework of a particular mental illness, each of these phenomenological variants of dementia acquires features of nosological specificity.
The beginning of the nosological taxonomy of acquired dementia was laid by E. Kraepelin (1909), who argued that there are as many forms of dementia as there are diseases with an unfavorable outcome. This position of Kraepelin was maintained and developed by a number of other psychiatrists, especially V.P. Osipov (1931) and I.F. Sluchevsky (1957).
Paralytic dementia.
Paralytic dementia differs among progressive paralysis. Being phenomenologically global, it has signs of nosological specificity. Against the background of growing sluggish complacency, euphoria, capriciousness and inactivity, the elements of the most complex, finely differentiated mental functions are lost, destroying the highest forms of social behavior. This manifests itself in a kind of forgetfulness, absent-mindedness (the patient may come to work in slippers), frivolity (skips on official duties, wastes money on trifles), in the loss of ethical skills (grabs the best pieces of food, can be cynical). Patients initially suffer from cognitive functions: “stupidity” appears, they do not immediately understand the questions asked to them, caution decreases, and criticism of their behavior and relationships with others decreases. Logically correct judgments and counting operations are lost. Quite often a megalomanic delusion of grandeur arises (magnificent, absurd, boundless, growing during the conversation). The speech of patients becomes uncertain, “smeared,” nasal, and trembling. Dysarthria, stumbling on syllables, logoclonia, permutations and omissions of syllables are detected. This is most pronounced during rapid speech and when pronouncing difficult words (“whey from yogurt,” “three hundred and thirty-third artillery brigade”). Characteristic handwriting disorder. Memory suffers: patients have difficulty remembering and reproducing information; there may be pseudo-reminiscences, paralytic (grossly absurd) phantasms. Patients confuse dreams with reality.
Higher feelings, especially the most complexly organized ones, such as feelings of shame, tact, and distance, decrease. Gradually, “dullness of spiritual feeling” appears: patients become indifferent to the troubles of relatives, sloppy, rude, cynical, and prone to violence when sexually aroused. There may be attacks of absurd psychomotor agitation. Typically trembling of fingers and tongue. There is coarsening of facial expressions, fibrillary twitching of the orbicularis oris muscles, and a mask-like face. Characterized by anisocoria, miosis, deformation of the pupils, sluggish reaction or lack of reaction of the pupils to light while maintaining it for accommodation and convergence - Argill Robertson syndrome (Argill Robertson D., 1869).
Pseudoparalytic dementia.
Pseudoparalytic dementia (Clippel M., 1891) is observed in syphilitic psychosis, vascular pathology, alcoholism, acute infection, and traumatic brain injury. Clinically, pseudoparalytic dementia is similar to paralytic dementia. There are memory impairments, weakening of cognitive functions, ingenuity, difficulties in associative processes, counting operations, combinatorial ability, as well as euphoria, delusional ideas of greatness, sometimes with elements of absurdity. There may be attacks of psychomotor agitation. There is trembling of the fingers, tongue, facial muscles, trembling of the voice, sluggishness of pupillary reactions. The most common are demented-euphoric and expansive variants of pseudoparalytic dementia.
In pseudoparalytic dementia caused by vascular pathology, along with the indicated signs, there is a flickering of clinical manifestations. During the period of episodic improvements, patients show a critical attitude towards their condition, and signs of personality preservation are revealed. The mood during this period becomes depressive. Quite typical in the vascular genesis of pseudoparalytic syndrome is the presence of asemic symptoms (aphasia, disorders of gnosis and praxis).
With the alcoholic origin of pseudoparalysis syndrome, its clinical structure also reveals signs of alcoholic personality changes (dominance of drinking habits, characteristic alcoholic humor, alcoholic psychological defense, alcoholic delusions of jealousy, etc.). Phenomena of polyneuritis often occur (from mild neuritic phenomena to paresis). The reverse development of psychopathological manifestations is characteristic when alcoholism stops.
Pseudoparalytic syndrome can be a stage of an acute exogenous reaction, followed by remission leading to asthenia (Bleikher V.M., 1976). However, it can be (for example, after a stroke) the onset of lacunar dementia.
Having reached the greatest degree of development, pseudoparalytic dementia usually regresses or takes a stationary course. Subsequently, especially when treating the underlying disease, persistent improvement and even recovery are possible.
Discirculatory dementia.
Dementia in vascular diseases of the brain (with cerebral atherosclerosis, hypertension and hypotension, after a stroke, with thromboangiitis - Vinivater-Buerger disease).
Phenomenologically, vascular dementia refers to lacunar dementia. The onset of vascular dementia (the most common is atherosclerotic) is characterized by the appearance of fatigue and a slowdown in all mental functions. Initiative disappears, it becomes difficult to get ready to do anything. Easily distractible. Memory impairment manifests itself mainly in poor memorization. Short-term memory - “note” - suffers especially (Bokiy I.V., 1969). Difficulties arise in reproducing the chronological order of events, proper names, and other names. In this case, the patient does not accept the incorrect hint, but he himself cannot immediately remember. After some time, the patient remembers what is necessary. The emergence of a tendency towards dissimulation of mnestic disorders is quite typical. Characteristic is an increase in depletion of mnestic functions. Memory deceptions (pseudo-reminiscences and confabulations) may occur. In some cases there may be a “shift into the past” (ecmnesia). As memory deteriorates, signs of amnestic disorientation, and subsequently amnestic confusion, appear. The latter is aggravated during episodic states of anxiety and restlessness. Against the background of mnestic disorders, asemic symptoms are often found in the form of verbal and literary paraphasias, amnestic aphasia, and elements of agraphia. These disorders are characterized by fluctuations in the intensity of manifestations, “flickering symptoms” (Stertz G., 1911). All this affects cognitive functions: the formation of judgments and inferences deteriorates. At first, inconsistent judgments appear. Then there is a characteristic decrease in the level of generalization and distraction, depending on the exhaustion of mental processes and therefore it can fluctuate. It is especially difficult to operate with abstract concepts.
At first, the patient, with pain in his soul, himself notices his mental insolvency. This is accompanied by a melancholy coloring of experiences, a feeling of emptiness in the soul. At the same time, basic skills, established relationships with people, moral attitudes and other personal manifestations remain intact for a long time, although they are usually accompanied by a sharpening of negative premorbid character traits. Patients are characterized by mood swings, emotional instability, and irritability. Subsequently, incontinence of emotions, faintheartedness, and sometimes involuntary crying appear. The deepening of dementia and the increase in focal symptoms lead to the phenomena of anosognosia, the disintegration of the personality core and the formation of a picture of global dementia.
Abashev-Konstantinovsky A.L. (1966) indicates the possibility of acute occurrence of persistent lacunar dementia syndrome after a stroke in patients who had not previously shown any manifestations of dementia.
Vascular dementia can be of the nature of amnestic (simple) dementia, amnestic-paramnestic (with Korsakoff syndrome), postapoplectic (with a “push-like” increase) dementia, pseudoparalytic, asemic and marantic dementia.
Hypertensive and hypotonic diseases, in the initial stages, are characterized by a narrowing of the attention span, increased exhaustion, easy involuntary switching, memory loss, emotional hyperesthesia, irritable weakness, and decreased intellectual productivity. Subsequently, with the development of discirculatory encephalopathy, dementia is formed, the structure of which reveals a sharp decrease in mnestic functions (forgetting the names of relatives and friends, facts of one’s biography, the collapse of logical-abstract memory), confabulation and pseudo-reminiscence, loss of professional skills, misunderstanding of abstractions, logical-grammatical constructions , cause-and-effect relationships, violation of counting operations, apratic-agnostic disorders, emotional dullness, apatho-abulic manifestations. There is an accentuation of negative premorbid personal characteristics, and then - selfishness, moral and ethical impoverishment, and often litigiousness. In hypertension, dementia progresses faster than in cerebral atherosclerosis. This is facilitated by frequent acute disorders of cerebral circulation, accompanied by the occurrence of focal lesions.
With endothromangiitis obliterans (Vinivater-Buerger disease), observed mainly in men, not only the vessels of the lower extremities, but also the vessels of the brain are often affected. In these cases we are talking about the cerebral form of the disease. Patients experience the so-called “intermittent claudication of the brain centers” (Déjérine JJ, 1906), manifested in transient disturbances of vision, speech, attacks of fear, twilight disorders of consciousness, etc. Dementia in cerebral obliterating endarteritis is lacunar (amnestic) in nature. Then it deepens quite quickly, asemic disorders increase, the core of the personality disintegrates, and signs of global dementia (pseudoparalytic or pseudotumorous type) form.
Traumatic dementia.
Traumatic dementia, like vascular dementia, belongs to the group of lacunar dementias. Typical of it are slowness, inertia and uncritical thinking (S.N. Davydenkov, 1938), combined with an overestimation of one’s own personality and a desire for monotonous and stereotypical reasoning. No less typical are pronounced mnestic disorders, exhaustion of them and cognitive functions in general, the predominance of specific judgments, difficulties in identifying essential features and in using abstract concepts. Characterized by irritability and emotional instability or an indifferent good-natured mood, in some cases accompanied by insufficiently targeted excessive activity, fussiness, or a decrease in volitional activity. With traumatic dementia, a peculiar reduction of attention is observed - the patient is affected as stimuli only by those objects that are in the field of vision (Gilyarovsky V.A., 1944). There is no clear correspondence between memory and intelligence defects, as is the case with epileptic and atherosclerotic dementia. With a moderately pronounced intellectual decline, a significant impairment of mnestic functions can be observed (Bleikher V.M., 1976).
There are two variants of traumatic dementia (Pivovarova V.L., 1965): simple traumatic dementia - with relative orderliness of behavior and with the manifestation of affective instability, and psychopathic traumatic dementia - with disinhibition of behavior, hysterical manifestations, as well as euphoria, foolishness and increased self-esteem. The first option includes cases of apathetic-abulic syndrome with symptoms of aspontaneity, lack of initiative, bradypsychism, torpidity, a decrease in the stock of information and skills, and impoverishment of speech. It is associated with damage to the convexity surface of the frontal lobe. Psychopathic-like traumatic dementia is associated with damage to the basal surface of the frontal lobe. And since traumatic dementia affects not only the frontal, but also the frontotemporal parts of the cerebral cortex (Povitskaya R.S., 1948), relatively often among its clinical manifestations there are asemic disorders (amnestic aphasia, alexia, agrammatism, etc. .). In some cases, mnestic disorders reach the level of Korsakov's syndrome. When the temporal lobe of the dominant hemisphere of the brain is damaged, pronounced personality changes are characteristic, manifested in a decrease in initiative, difficulties in using life experience, frivolous actions, apathy, and sometimes depressive-dysphoric disorders (Landolt H., 1960). With the progressive course of traumatic dementia, uncritical self-esteem reaches such a degree that we can talk about pseudoparalytic dementia (Bleicher V.M., 1976).
One of the variants of post-traumatic dementia syndrome is “puerile traumatic dementia” described by Busemann (Busemann A., 1950). It is characterized by a combination of dementia with the phenomena of puerilism, carelessness, deliberate childishness, a violation of the logical structure of thinking, consistency, insufficiency of the interconnectedness of judgments and the correspondence of their perceived reality.
V.A. Gilyarovsky (1946) points to the possibility of post-traumatic mental disorders of the type of pseudo-organic dementia, in which signs of severe intellectual deficiency are observed, but they are reversible.
Epileptic dementia.
Epileptic dementia has certain similarities with traumatic dementia. In particular, this is revealed in the presence of bradypsychia and inertia. However, in contrast to traumatic and vascular dementia, with epileptic dementia the pace of mental activity, although slowed, is uniform - there is no increased exhaustion (Bleikher V.M., 1976), the slowdown of mental processes is combined with bradykinesia and oligophasia. Concrete thinking predominates, which is not only stiff, but also viscous, which is manifested in the tendency of patients to be excessively thorough, detailing, and in their difficulty in separating the main from the secondary. Patients in their judgments cannot be distracted from the details, “treading water,” but they do not lose the purpose of the statement. Their speech is replete with patterns, characterized by a peculiar floridity, the use of diminutives and endearments, and primitive rhyming. There is a tendency to embellish speech. “Reasoning” and instructive statements are characteristic, reflecting the tendency of patients to be somewhat pathetic and overestimate their own life experience. Patients love to give instructions, teach, sometimes becoming the role of an “unpleasant, narrow moralist” (Sukhanov S.A., 1912). The patients’ statements are shallow, superficial, and contain banal associations. There is a gradually increasing depletion of vocabulary - progressive oligophasia (amnestic-aphasic complex according to A.N. Bernstein). A combination of instructiveness, oligophasia and egocentric tendencies is typical. The latter are manifested in a constant desire to “include oneself in the situation” (Zavilyansky I.Ya., Tarashchanskaya R.E., 1959), in attempts at self-affirmation, in a thirst for recognition. With epileptic dementia, memory decreases, and there is a parallelism between the severity of dementia, oligophasia and memory impairment. The egocentric affective-personal orientation of thinking processes gives epileptic dementia special features that allow it to be defined as concentric (Sluchevsky I.F., 1957). It is characterized by a narrowing of the patient's interests in his own personality, a narrow range of thinking, a decrease in the level of generalization and distraction, loss of a sense of humor (this is due to slow-wittedness and difficulty identifying the essential). The overestimation of unimportant signs that is often observed in epileptic dementia makes it necessary to differentiate it from schizophrenic dementia, in which there is an actualization of “weak” signs and the destruction of stereotypes and patterns.
There are several types of epileptic dementia: simple dementia, characterized by progression and the absence of productive psychopathological symptoms; viscous-apathetic dementia, in which pronounced apathy, slowness and stiffness of intellectual and emotional manifestations, lack of affective tension and explosiveness are revealed (Morozov V.M., 1967). Similar signs, as well as pronounced phenomena of oligophasia, are described by Ya.P. Frumkin, I.Ya. Zavilyansky (1964) in the structure of the inert-oligophasic variant of epileptic dementia. Paranoid epileptic dementia includes productive psychopathological symptoms, in particular, systematized paranoid and paraphrenic experiences. It is characterized by a protracted course and relative intellectual-mnestic preservation. Pseudoparalytic dementia is relatively rare, the distinctive features of which are less mobility, concreteness of delusional ideas of grandeur, poorer in content than with progressive paralysis. In addition, against the background of a complacent-euphoric affect, explosiveness occasionally manifests itself.
According to epidemiological studies, epileptic dementia occurs in approximately 20% of cases of epilepsy (Kerbikov O.V., 1947). It is of interest that in patients with epilepsy with premorbid high intelligence, dementia is detected later and to a lesser extent.
Senile dementia.
Senile dementia is phenomenologically related to global dementia. It usually begins after 65 years. Noteworthy is the decrease in mental activity, which acquires the features of rigidity. Personality changes are typical in the form of ever-increasing manifestations of patients’ egocentrism, their indifference to loved ones, unmotivated stubbornness, stinginess, sometimes pedantry, and a suspicious attitude towards the environment.
Against the background of the rapidly growing gross destruction of both the intellect itself and its prerequisites, signs of moral dullness and destruction of the core of the personality are revealed. Violations of both semantic and mechanical memory rapidly progress in accordance with Ribot's law (Ribot Th., 1881): first for current events, then for events of the recent past, and so on. Affectively significant events are retained in memory the longest. A certain vividness of affectively colored memories is possible - “affective emboli” (Bleikher V.M., 1976). Amnestic disorientation with manifestations of ecmnesia is typical: patients cannot name the date, day of the week, year, season, do not know their location, often greatly reduce their age (“18-20 years”), women give their maiden name, etc. This determines the appearance of a characteristic “shift of the situation into the past.” The phenomena of fixation amnesia arise quite quickly (patients are not able to remember new material). False recognitions that occur often also reveal an ecmnesic tendency: strangers are perceived as relatives and friends who surrounded the patient in his youth. At later stages of the disease, amnestic aphasia phenomena are observed.
From the very beginning, the processes of generalization and distraction suffer, and patients quite quickly cease to cope with the simplest intellectual tasks - they cannot find generalizing names for several objects, exclude similar features, etc. Lost interest in the environment.
At the beginning of the disease, patients experience a constant desire to communicate with others and talkativeness. However, the increasing semantic impoverishment of the patients’ speech, impaired understanding of speech addressed to them and their rapid loss of the thread of the conversation make communication unproductive. However, patients can have a “conversation” without an interlocutor. When they lose the topic of conversation, patients often turn to topics from old life situations (Vaisbord S.A., 1959). Unlike atherosclerotic dementia, liveliness and naturalness of speech are preserved for a long time (Zhislin S.G., 1956). Along with verbosity, there is a progressive depletion of vocabulary, stereotypical repetition of phrases, perseveration, and verbal paraphasia. Gradually, the speech of patients becomes increasingly fragmented, turning into an incomprehensible set of words (verbigation), into inarticulate muttering.
Praxis disorders appear much later than oral language disorders (unlike Alzheimer's disease). This is most expressed in the phenomena of agraphia: handwriting is disrupted - letters become angular, then turn into scribbles and monotonously repeating strokes (senile agraphia according to Kraepelin).
There are several variants of senile dementia. Simple senile dementia is characterized by gradually increasing intellectual decline, general progressive amnesia, loss of mental activity, emerging disintegration of the personality core, and moral dullness. Senile dementia with agitation and confabulations - chronic presbyophrenia (Kahlbaum K., 1863; Wernicke C., 1881) includes, along with typical senile personality changes, mnestic disorders with a shift of the situation into the past, amnestic disorientation and confabulations, the development of dementia, hypomanic manifestations: elevated euphoric mood, increased fruitless activity, talkativeness, exaggerated politeness, verbosity, accelerated speech with symptoms of distractibility.
When vascular disorders are added to the senile-atrophic pathology, the picture of the disease acquires the features of Alzheimer's syndrome - Hackebusch-Geyer-Geimanovich disease (Hackebusch V.M., Geyer T.A., Geymanovich A.I., 1912, 1916).
⇐ Previous18Next ⇒
Diagnosis of dementia
If characteristic symptoms of dementia appear, you should consult a neurologist. During a personal visit, a specialist will study your medical history and conduct an examination. Testing mental abilities is a mandatory procedure. The doctor will ask the patient several questions to find out how well the person is oriented in time, space, what he remembers and how he thinks.
To exclude diseases associated with dementia, urine and blood tests may be prescribed. Psychiatrists and gerontologists also work with older people. Due to their experience, they can assess the patient’s condition and prescribe supportive drug therapy. For a detailed memory test, the patient is prescribed an MRI or CT scan. The procedure can detect signs of Alzheimer's.
Difficulty completing routine tasks
The appearance of difficulties in performing familiar tasks may be an early sign of the onset of dementia. As a rule, it all starts with the fact that a person cannot perform complex tasks: check the balance of a credit card or remember the rules of a game. Additionally, you may notice that a person nearing retirement age has a hard time doing new things or following new rules.
How your date of birth determines the rest of your life
What do people regret most at the end of their lives?
14 ways to find out about a cat's attitude towards itself
Dementia treatment
Senile dementia cannot be cured. Medications can correct the patient’s behavior and temporarily improve his condition. Medicines are prescribed depending on the type of course and severity of the disease. To reduce the manifestation of dementia, the patient is prescribed medications based on galantamine.
This category of medicines:
- has a neuroprotective effect, preventing the destruction of brain cells;
- helps improve nerve impulses;
- restores memory and cognitive abilities.
To correct behavioral disorders, the patient is prescribed to take antipsychotics. Medicines in this category eliminate psychomotor agitation and delirium. Drugs such as Haloperidol have many side effects. To relieve the patient of depression, medications based on fluoxetine are prescribed. To normalize sleep, take sleeping pills.
Warning Sign #2: Difficulty finding words.
Difficulty remembering words is another sign of dementia.
It looks as if the speaker is trying to remember a word, but cannot find it.
And these are not necessarily fancy or very specific words. This can happen with words that you use many times a day.
This slows down conversations and also indicates problems with the language centers of the brain.
Tips for developing early symptoms of dementia
Behavioral disorders that occur in the early stages of senile dementia can be corrected without resorting to drug therapy.
Experts recommend that older people reconsider their usual lifestyle.
Lots of movement
An effective method that allows you to restore previously lost skills is regular physical education.
Outdoor workouts:
- contribute to the normalization of metabolism within tissues;
- accelerate the process of formation of synaptic connections;
- support vital activity at the cellular level.
Active dancing and play sports will allow the patient to get rid of irritability and fatigue.
Communication with people
Patients suffering from senile dementia need to communicate regularly with others. This is the main condition for the social and mental development of a person.
By establishing contact with relatives, friends, neighbors and acquaintances, the patient develops his inner self and shapes himself as an individual. With dementia, the patient loses the ability to interact with others. There is no logic in the reasoning, mood swings and other personality changes are observed.
To help an elderly person restore communication, it is necessary to learn to hear and listen to the patient. If the patient is not able to independently choose the right word in a conversation, then you can ask him leading questions or try to build a logical chain with him.
People suffering from senile dementia see the surrounding reality distorted. You cannot impose your opinion on the patient or actively convince him.
Brain training
Brain training allows you to restore logical thinking, analytical and visual memory.
The patient can be offered:
- try to arrange things by size and color;
- find pictures in the book that depict a specific person, plant or animal;
- write down a few words from dictation;
- finish a proverb or saying;
- identify a fruit, vegetable or spice by touch.
To develop fine motor skills of the hands, the patient is asked to sculpt some figure out of plasticine.
To give up smoking
Smoking can cause constriction of blood vessels in the brain. If blood flow is disrupted, the risk of developing hypoxia is quite high. People suffering from senile dementia (regardless of the type and stage) need to completely stop using tobacco products.
Proper and long sleep
It is important for older people to get proper rest. Night sleep should last at least 8 hours - during this time the body has time to restore the energy spent. Long rest allows the brain to “unload”, the organ again gets the opportunity to correctly process the information received. Lack of sleep negatively affects not only the physical, but also the mental state of the patient.
Diet
Together with food, the human body receives a large amount of vitamins, micro- and macroelements necessary for the normal functioning of cells. An unhealthy diet, frequent snacking or partial refusal to eat can cause disturbances in the functioning of the digestive system.
During the rehabilitation period, the patient must adhere to a therapeutic diet.
List of prohibited and permitted products:
| Category | Allowed | Prohibited |
| Vegetables | Pumpkin, zucchini, beets, cabbage, carrots. | Radish, radish, onion, garlic. |
| Fruits | Tangerines, lemons, apples, pears, avocados. | Peaches, pomegranate, pineapple, grapes, melon. |
| Cereals | Barley, semolina, buckwheat, millet. | Rice (except brown), lentils. |
| Meat and fish | Lean veal, poultry (turkey, chicken), rabbit. | Fatty meats (beef, lamb). |
| Sweets | Jam, preserves, fruit marmalade (sugar-free), baked goods. | Chocolate, liqueur candies, pastries with rich cream, cakes. |
| Sausages and smoked meats | Chicken sausage, boiled sausage, ham. | Smoked fish, fatty boiled pork, smoked lard. |
| Beverages | Freshly squeezed fruit and vegetable juices, green tea, herbal infusion, cocoa. | Alcoholic drinks (including low alcohol), strong coffee, black tea. |
If a person forgets to eat, then he needs to be carefully reminded about it. It is better to feed the patient when he is in a good mood. The diet should consist of semi-liquid and liquid foods, especially if the patient has problems swallowing. It is better to find out the patient’s gastronomic preferences in advance and prepare food in accordance with them.
Prevention of vitamin deficiency
To prevent vitamin deficiency, you need to eat a balanced diet and include more vegetables and fruits in your diet. You can take vitamin complexes prescribed by your doctor. Independent selection of dietary supplements is strictly prohibited: an excess of minerals or vitamins caused by taking an “inappropriate” drug can aggravate the situation.
Dementia in adults is a pathology that is diagnosed in every 5 elderly people. Symptoms appear gradually, and many people do not pay attention to them in time. The occurrence of delusions, hallucinations, memory and speech disorders is a reason to contact a medical institution.
Prevention measures
It is possible to prevent the development of vascular dementia if you prevent any cerebrovascular diseases, and if they occur, carry out adequate therapy to prevent progression. If you have atherosclerosis and hypertension, it is recommended to follow a healthy diet with low cholesterol levels, and also adhere to a healthy lifestyle in general.
If a patient has suffered a stroke, it is extremely important to follow all doctor’s recommendations during the rehabilitation period and throughout the subsequent years of life. Self-training of your own mind will be of great benefit. You need to read as much as possible, memorize, try to retell passages of texts or learn them by heart.
Warning Sign #7: Problems with time perception.
For such people, minutes, days and years seem the same, and the passage of time suddenly becomes meaningless.
If you notice that what's going to happen in an hour, or tomorrow, or next week doesn't seem to mean anything to the person, it may be a sign that their sense of time has changed.