Epilepsy is a serious neurological disease, the causes of which in adolescents (boys and girls) are different, as are the symptoms for which treatment is prescribed.
The disease has a genetic predisposition, but manifests itself at different periods of life under the influence of external factors that serve as an impetus for the development of the process. It may awaken in infancy, or maybe at 17 years old and later.
With timely treatment, children can live a full life without suffering from severe attacks. In some cases, after 1-3 years of treatment, the diagnosis is removed.
Prognosis and prevention
Adolescent epilepsy is considered a chronic disease.
Spontaneous remission is rare. In 90% of patients who interrupted treatment, epileptic attacks return, but in some cases a long period of remission is observed. When proper treatment is prescribed, in 80% of cases it is possible to completely rid the patient of seizures. The drugs are discontinued gradually over several years. This is done in order to completely eliminate relapse.
Juvenile epilepsy does not affect mental abilities in any way, so there is no need to worry about the child’s development.
Prevention consists of taking actions to prevent the occurrence of epileptic seizures.
This requires:
- Timely diagnosis of chromosomal syndromes and various hereditary diseases.
- Careful examination of pregnant women who are at high risk of giving birth to a child suffering from epilepsy. Most often this applies to women who take drugs and suffer from endocrine disorders.
- Observation of children who were underweight at birth or had other deviations from the norm.
- Conducting social events for patients with juvenile epilepsy.
Timely, competent diagnosis increases the chance that treatment will be effective. At the first suspicion of epilepsy, a child should be shown to a doctor.
He will develop an individual treatment plan. Its strict adherence guarantees a cure in most cases, so there is no need to despair.
About epilepsy in adolescents in this video:
Forecast
Treatment of epilepsy in adolescents and its causes comes down to complex therapy, which is calculated individually in each case. This necessarily includes taking anticonvulsants (usually one medicine).
Spontaneous remission after treatment occurs only in 10% of cases . In 90% of patients who interrupt therapy, the disease recurs. Periods of remission up to several years are possible. If therapy is prescribed correctly, then a teenager is relieved of seizures in 80% of cases. Mild and moderate epilepsy does not affect mental abilities in any way.
Guide for Parents
M.Yu. Nikanorova, E.D. Belousova, A.Yu. Ermakov
Compiled by:
Head of the Department of Psychoneurology and Epileptology of the Moscow Research Institute of Pediatrics and Pediatric Surgery of the Ministry of Health of the Russian Federation, Head of the Children's Scientific and Practical Anticonvulsant Center of the Ministry of Health of the Russian Federation, Doctor of Medical Sciences, Professor Marina Yuryevna Nikanorova.
Leading researcher at the Department of Psychoneurology and Epileptology of the Moscow Research Institute of Pediatrics and Pediatric Surgery of the Ministry of Health of the Russian Federation, Candidate of Medical Sciences Elena Dmitrievna Belousova.
Senior Researcher of the Department of Psychoneurology and Epileptology of the Moscow Research Institute of Pediatrics and Pediatric Surgery of the Ministry of Health of the Russian Federation, Candidate of Medical Sciences Alexander Yurievich Ermakov.
Published with the support of Sanofi-Sintelabo
Dear parents!
This brochure is addressed to those who have a child in the family who suffers from epilepsy. If your child experiences epileptic seizures, you should, of course, consult a doctor. However, as practice shows, after the first consultation, parents still have many questions regarding the provision of emergency assistance in the event of an attack, treatment and prospects for the child’s further development. We hope that in this brochure you will find answers to your questions.
TABLE OF CONTENTS
Causes of epilepsy
The causes of epilepsy in adolescents are associated with pathological functioning of neurons. Due to the spread of impulses across both hemispheres, seizures occur. Parocrises - convulsive seizures - occur between the ages of 11 and 17, and become more intense in adulthood.
In some cases, epilepsy goes away with age, especially in mild cases.
For reasons in adolescents, the disease is divided into 3 degrees:
- Idiopathic. Teenage epilepsy is passed on from parents.
- Secondary. Occurs as a symptom of complications after severe infections and injuries affecting the brain or nervous system. Sometimes it develops due to neoplasms.
- Cryptogenic. The diagnosis is made if no other obvious causes are found.
Cells begin to work incorrectly due to external factors and internal characteristics of adolescence. So, the impetus can be hormonal changes. And sometimes the cause is a failure that occurred during intensive development.
The psychological and emotional state of the child is no less important. The cause of epilepsy in adolescence can be severe stress caused by an unfavorable atmosphere in the family or excessive stress placed on the teenager. Sometimes the cause is teenage quarrels. Other reasons:
- trauma – mainly as a result of severe TBI, epilepsy attacks develop (including several years after the injury);
- organ diseases, including infantile paralysis, vascular pathologies in the brain;
- metabolic problems - in 10% of cases, adolescents have congenital or acquired pathologies (diabetes, lead poisoning, obesity due to abuse of unhealthy foods).
The disease can also be triggered by long-term exposure to toxic substances, including medications and drugs.
Types of disease
Depending on the pathogenesis, epilepsy in childhood is differentiated by specialists into three groups:
- idiopathic: stated if the symptoms of the disease appear as a result of a genetic factor, but without significant pathologies in the brain;
- symptomatic: considered a consequence of brain defects due to developmental anomalies, injuries, neoplasms;
- cryptogenic: recorded by doctors in cases where the disease appeared due to unidentified causes.
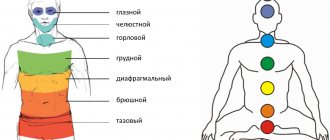
Symptomatic epilepsy in children differs in the area of localization of the pathogenic focus.
And depending on its location, it manifests itself in several types:
- frontal;
- parietal;
- temporal;
- occipital;
- chronic progressive.
The listed types of epilepsy manifest themselves in different ways. For example, frontal occurs only at night; For the temporal lobe, blackouts of consciousness without pronounced convulsive symptoms are characteristic.
Finding out the causes of the disease and its type helps to choose an adequate line of combating it. However, this is not enough for successful treatment: it is important to promptly recognize the first signs of epilepsy in a child.
Symptoms of epilepsy
With epilepsy, all symptoms occur spontaneously, less often provoked by bright flashing lights, loud sounds or fever (increased body temperature above 38C, accompanied by chills, headache and general weakness).
- Manifestations of a generalized seizure include generalized tonic-clonic seizures, although there may be only tonic or only clonic seizures. The patient falls during a seizure and often suffers significant injuries; very often he bites his tongue or loses urine. The seizure usually ends in epileptic coma, but there is also epileptic excitement, accompanied by twilight darkness of consciousness.
- Partial seizures occur when a focus of excessive electrical excitability forms in a specific area of the cerebral cortex. Manifestations of a partial attack depend on the location of such a focus - they can be motor, sensitive, vegetative and mental. 80% of all epileptic seizures in adults and 60% of seizures in children are partial.
- Tonic-clonic seizures. These are generalized convulsive seizures that involve the cerebral cortex in the pathological process. The seizure begins with the patient freezing in place. Next, the respiratory muscles contract, the jaws tighten (the tongue may be bitten). Breathing may be cyanotic and hypervolemic. The patient loses the ability to control urination. The duration of the tonic phase is approximately 15-30 seconds, after which the clonic phase begins, during which rhythmic contraction of all muscles of the body occurs.
- Absence seizures are attacks of sudden blackouts for a very short time. During a typical absence seizure, a person suddenly, for absolutely no apparent reason either for himself or for those around him, stops responding to external irritating factors and completely freezes. He does not speak, does not move his eyes, limbs or torso. Such an attack lasts a maximum of a few seconds, after which it also suddenly continues its actions as if nothing had happened. The seizure remains completely unnoticed by the patient himself.
In a mild form of the disease, seizures occur rarely and are of the same nature; in a severe form, they are daily, occur 4-10 times in a row (status epilepticus) and have a different character. Patients also experience personality changes: flattery and softness alternate with malice and pettiness. Many experience mental retardation.
What causes
What are the causes of epilepsy and how do you get it?
Epilepsy can be caused by various factors:
- Psychosomatic - a seizure occurs due to the excitation of nerve cells in a certain part of the brain. The body ceases to obey the person, it shudders convulsively. What causes the development of epilepsy in this case? An attack can be triggered by constant violence against one’s own personality, denial of one’s right to life, or struggle with the outside world. The patient is in constant opposition, so strong that it leads to the development of a serious illness. Often the psychosomatics of the problem lies in childhood: if the child was suppressed as an individual, he may subsequently develop epilepsy.
Traumatic - after an injury, signs of epilepsy appear within a couple of weeks. They indicate damage to the cerebral cortex. At this time, early attacks occur, late ones are a reaction to possible hemorrhages that were not noticed by specialists earlier. With epilepsy after a head injury, patients may experience partial seizures accompanied by loss of consciousness.
Epilepsy after stroke. Why does epilepsy occur during a stroke? A weakened body is not able to cope with its consequences. An epileptic attack after a stroke occurs due to the formation of a post-stroke cyst, the formation of a tissue scar, or atrophy of certain areas of the cerebral cortex.
Alcohol abuse is associated with toxic tissue poisoning. Why does epilepsy occur in alcoholics? Epilepsy in this case develops more often if the patient suffers from atherosclerosis, has suffered a traumatic brain injury in the past, a serious infectious disease, or has a hereditary predisposition.
The epileptic gradually degrades, becomes embittered, touchy, absent-minded, his sleep is disturbed and his speech is distorted.
Meningitis. Why does epilepsy appear in this case? Convulsions occur due to ischemia of brain tissue and insufficient blood supply to this organ. The first seizures usually appear 3-4 days after the onset of the disease.
Hereditary predisposition - such patients have a special functional state of neurons. What causes epilepsy? They have a tendency to generate electrical impulses and excite. This feature is encoded in their genes. It is passed on to each subsequent generation. If a person is influenced by risk factors, the predisposition develops into a disease.
Treatment of epilepsy
The goals of treatment are to stop epileptic seizures with minimal side effects and to manage the patient so that his life is as full and productive as possible.
The patient and his family should receive instructions about taking the drug and be informed both about the actually achievable results of treatment and about possible side effects.
Principles of treatment of epilepsy:
- Compliance of the drug with the type of seizures and epilepsy (each drug has a certain selectivity in relation to one or another type of seizures and epilepsy);
- If possible, use monotherapy (use of one antiepileptic drug).
Antiepileptic drugs are chosen depending on the form of epilepsy and the nature of the attacks. The drug is usually prescribed in a small initial dose with a gradual increase until the optimal clinical effect occurs. If the drug is ineffective, it is gradually discontinued and the next one is prescribed. Remember that under no circumstances should you change the dosage of the medicine or stop treatment on your own. A sudden change in dose can provoke a worsening of the condition and an increase in attacks.
Drug treatment is combined with diet, determination of work and rest schedules. For patients with epilepsy, a diet with a limited amount of coffee, hot spices, alcohol, salty and spicy foods is recommended.
On the road to healing
To the question of whether epilepsy in children can be treated, today's medicine gives a positive answer. The success of therapy depends both on the professionalism of the doctors and on the attitude of the parents.
The latter must be prepared for the fact that it will take a long time to treat epilepsy in a son or daughter, without interrupting the course even for a day.
What is required from parents:
- provide the baby with a diet with limited fluid and salt;
- organize a rational daily routine with leisure breaks;
- eliminate stressful situations;
- limit your child’s access to TV and computer;
- make it a habit to walk in the fresh air, but avoid prolonged exposure to the sun or independent swimming in a pond or bath;
- Encourage your child to play safe sports: badminton, tennis, cross-country skiing, etc.
During a seizure, you need to place the baby on his side in a safe place. You cannot restrain convulsions, unclench your jaws, or give medicine or water. The main task of the parents of an epileptic is to prevent him from harming himself.
Drug treatment of epilepsy in children is determined taking into account the age characteristics and condition of the patient. The main role is given to anticonvulsants.
It is recommended to take them with a gradual increase in dose. When the number of attacks decreases and their intensity decreases, the full age dosage is prescribed.
In the symptomatic form of the pathology caused by a tumor in the brain, the patient can be cured surgically. Before the operation, a consultation of a neurosurgeon, neurologist and psychotherapist gathers, the risks of invasive intervention and the opinion of the parents are taken into account.
If the danger of the operation is too high, the question is “how to treat the patient?” decided in favor of drug therapy.
Diagnostics
Myoclonic symptoms are included in the clinical picture of many diseases and epileptic syndromes. The diagnosis of “myoclonic epilepsy” is established only when myoclonic seizures predominate over other clinical manifestations. Diagnostics is aimed at verifying the nosological form of epilepsy, and when identifying the secondary nature of myoclonus, at searching for the underlying pathology. The main diagnostic steps are:
- Collection of anamnestic data. The age of onset, the nature of the onset, and the order of development of symptoms are of great importance.
- Neurological examination. Conducted by a neurologist, it is aimed at identifying myoclonic contractions, focal deficits, determining the level of mental development, the degree of cognitive impairment, and assessing mental status.
- Electroencephalography. In most patients, diffuse interictal symmetrical epileptogenic discharges and ictal high-amplitude spikes are recorded. In some cases, to detect epiactivity, daily EEG monitoring and provocative tests (EEG with flashes of light, hyperventilation, sharp sound signals) are required. The research results are assessed by a neurophysiologist and epileptologist.
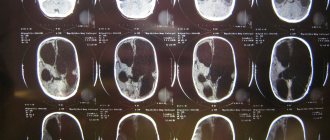
- Neuroimaging. Before the fontanelles close, it is carried out using neurosonography, in children over one year old - using MRI of the brain. Adults can undergo MSCT. Morphological changes in cerebral tissues are characteristic of symptomatic ME.
- Laboratory research. Performed if metabolic disorders are suspected. Includes biochemical analysis of blood and urine, specific tests.
- Genetic consultation. Collecting a family history and drawing up a family tree makes it possible to determine the hereditary nature of epilepsy and establish the type of inheritance.
Differential diagnosis is carried out with non-epileptic myoclonus, the distinctive feature of which is the focal nature of myoclonus, lack of response to provocation, and a normal EEG pattern. Differentiation of ME is also necessary with convulsive syndrome of infectious etiology, febrile seizures, Lennox-Gastaut syndrome, cerebellar myoclonic dyssynergia of Hunt.
Seizures in a child: causes, diagnosis, treatment
Thoughts will be filled with memories of terrible pictures of convulsions of patients with epilepsy. But the stress will pass, everything will fall into place. As soon as the baby feels better, you can calmly figure out the reasons for what happened.
Mechanism of occurrence and causes
Cramps are involuntary muscle contractions that occur under the influence of too much excitation of neurons in the motor part of the brain. They mainly appear in children under 3 years of age. With age, their frequency decreases. Convulsive activity remains in only 2-3% of children diagnosed with epilepsy or organic damage to the central nervous system.
A favorable condition for the occurrence of spasms is the unformed central nervous system of babies. Unpreparedness for full functioning after birth is common to all babies.
However, hypoxia during intrauterine development, intoxication and infectious diseases of the expectant mother lead to the fact that the immaturity of the brain structure and its functions in the newborn will be more noticeable.
Asphyxia, damage to the central nervous system, and hemorrhages that occur during childbirth also have a negative impact on the baby’s readiness for independent life. Most problems are corrected in the first year of life under the influence of drug therapy and physiotherapy.
The main causes of involuntary muscle spasms are:
- Traumatic brain injuries.
- Various types of intoxication.
- Vaccination.
- Epilepsy. The disease is mainly hereditary. It is believed that it is passed on through generations to children of the same sex.
- Inflammatory infectious diseases of the brain, for example, meningitis, encephalitis.
- Neoplasms.
- Congenital and acquired pathologies of the cardiovascular and endocrine systems.
- Heat. The threshold for responding to hyperthermia is different in different children and depends, among other things, on the formation of the central nervous system.
- Imbalance of vitamins and minerals.
Kinds
Seizures in children are classified according to several criteria:
- area of distribution;
- nature of tension;
- features of the course;
- reasons for occurrence.
Classification by area of distribution
Depending on the area of distribution, they speak of partial and generalized seizures. Partial (local) occur when the electrical activity of a certain area of the cerebral cortex increases. They manifest themselves as twitching of individual muscles of the foot, arms, tongue, including during sleep.
Generalized convulsions take over the entire body. A characteristic sign is the tension of the torso.
In this case, the head is thrown back, the legs are straightened, the arms are bent to the chest, the teeth are clenched, the pupils do not react to light, the skin turns pale and blue. In most cases, loss of consciousness occurs.
This is typical for epileptic seizures, hysteria, tetanus, acute intoxication or infection, and cerebral circulatory disorders.
Before an attack, hallucinations may appear; convulsions are immediately preceded by an inarticulate cry. With epilepsy, several seizures occur in a row. One attack lasts up to 20 seconds.
Classification according to the nature of voltage
Depending on the nature of the manifestation, they speak of clonic, tonic and atonic seizures. Clonic spasm is pulsating in nature, the muscles contract and then relax. Chaotic movement of the limbs is characteristic.
The baby may wake up and cry. Tonic cramps are characterized by strong, prolonged muscle tension. The limbs seem to freeze for an indefinite period of time. Appear slowly. The baby doesn't make a sound.
There are also tonic-clonic convulsions.
This group of seizures includes atonic ones. They are characterized by a lack of tension. All muscles quickly relax. Involuntary bowel movements or urination may occur. Often the cause of atonic spasms is Lennox-Gastaut syndrome, which manifests itself in children aged 1 to 8 years.
Classification according to flow characteristics
Depending on the characteristics of the development of seizures, they speak of myoclonic, flexor, infantile spasms and absence.
Myoclonic spasms occur in infants and instantly involve one or more muscles. Does not cause pain. From the outside they resemble tics or twitching. The main causes are metabolic disorders and brain pathologies. The attack lasts for 10-15 seconds.
Infantile convulsions during sleep in a child aged 6-12 months. Occurs during sleep or after waking up due to sudden movements and during feeding.
They manifest themselves as a scream, a grimace, rolling of the eyes, an increase in the size of the pupils. It is believed that seizures in children of this type are evidence of mental retardation.
They may also be the initial symptom of paralysis, microcephaly or strabismus.
Flexor spasms are typical for children under 4 years of age. Unrelated flexion or extension of the body, neck, and limbs occurs, repeated several times. Duration - from a few seconds to half an hour. Loss of consciousness may occur for a short time. The causes are unknown.
In children aged 4 to 14 years, absence seizure develops, characterized by stopping gaze, lack of response to external stimuli, and immobilization. In some cases, involuntary chewing movements and smacking occur. This is due to stress, fatigue, traumatic brain injury, and brain infections. According to EEG data, electrical activity increases in the occipital region.
Classification by causes
The most common types of seizures in children are febrile, epileptic and respiratory-affective seizures.
Febrile convulsions in a child occur before the age of 6 years with the highest frequency of occurrence between the ages of 6 and 18 months. Once occurring, convulsions with fever appear in 30% of children.
The pathology covers both single muscles and individual groups. Possible facial tension and tilting of the chin. The skin turns blue, the baby sweats a lot.
At some point, loss of consciousness and cessation of breathing may occur. Then comes relaxation.
Without fever, convulsions occur in a child due to epilepsy. In this case, the attack is generalized.
Respiratory-affective symptoms arise due to an excess of emotions in children from six months to 3 years. Characteristic of premature babies.
Symptoms
The main signs of seizure activity are:
- involuntary movements;
- cyanosis of the skin;
- limb tension;
- tightly clenched teeth;
- foaming;
- involuntary urination;
- eye rolling.
Diagnostics
Even after a single attack, it is important to conduct a diagnosis and understand the question of why the convulsions occurred. This will allow you to avoid relapse, prescribe treatment and simply calm down. Seizures can occur not only with fever and epilepsy. In infants, they may be the first signs of cerebral palsy or mental retardation.
After recovery, the pediatrician gives a referral for tests and a visit to a neurologist or endocrinologist. Tests include a general picture of urine, blood and biochemistry. In most cases, you will need to do an electrocardiogram and consult a cardiologist.
The pediatrician and neurologist will take a history of the attack by asking questions about the following:
- heredity;
- what could have caused the attack;
- features of pregnancy and childbirth;
- features of the first year of life;
- attack duration;
- symptoms;
- the nature of the seizures;
- how many times the spasms were repeated;
- whether there was a loss of consciousness.
In some cases, the neurologist will send you for a so-called lumbar puncture - a sample of cerebrospinal fluid. An electroencephalogram is required. If neoplasms or vascular disorders are suspected, the doctor gives directions for an ultrasound of the brain and neck, MRI or computed tomography. A fundus examination and consultation with an ophthalmologist may be required.
Seizures with fever also require diagnosis, despite the fact that the cause of their occurrence seems clear. Only 5% of young children develop convulsive attacks during hyperthermia, so it is better to make sure that the child does not have any organic pathologies.
First aid
When the first signs of a seizure occur in children, regardless of their cause, emergency assistance must be called. Often parents have no idea what to do when their child has seizures.
In case of convulsive activity of any etiology, remove all dangerous objects that could lead to injury to the patient. If an attack occurs indoors, open a window for ventilation.
The temperature in the room should not be higher than 21 °C.
Adults, be they parents, caregivers or teachers, must constantly remain with the patient until the attack is completely over and consciousness returns.
In all cases, when joining convulsions, stopping or holding your breath, you must remember that during an attack it is impossible to perform artificial respiration. The muscles of the respiratory tract are tense and do not allow air to pass through. You need to wait for the attack to end. It is not recommended to wake up or disturb the patient.
As first aid for convulsions in children, they are laid on a hard surface, the whole body or just the head is turned on its side, and outer clothing is removed or loosened. Under no circumstances are you given anything to drink. As soon as the cramps go away, saliva and vomit are removed from the mouth.
If a seizure begins in a child diagnosed with epilepsy, you must be prepared for the spasms to cover the entire body. They will be accompanied by loss of consciousness, and perhaps a second attack will occur.
After the child is laid down, a towel roll is placed under the neck, and a corner of the towel is inserted between the molars. Under no circumstances should a metal object be placed in the mouth; it can damage the teeth, the remains of which will fall into the larynx.
Any medications are administered intramuscularly and only by a doctor.
Why do infants experience seizures: causes and consequences
If convulsions occur in children at high temperatures, they are undressed, wiped with alcohol, and covered with a towel dipped in water.
During an attack, it is unacceptable to give medications orally. The muscles are compressed, the baby still won’t swallow it, but he will be able to choke on it after the attack is over.
If it is necessary to urgently take measures to reduce the temperature, rectal suppositories with paracetamol are given.
Treatment
Therapeutic tactics depend on the nature and causes of the disease.
In case of seizures with fever or convulsions of an affective-respiratory nature, children are usually not hospitalized; treatment continues at home.
After the attack caused by the high temperature has ended, children are re-cooled by wiping the body with a solution of vinegar, vodka or applying a damp towel to the forehead. If after the end of the convulsions the temperature does not subside, the baby is given an antipyretic - Paracetamol or Efferalgan.
If attacks recur or last for more than 15 minutes, the doctor prescribes anticonvulsants - Diazepam or Phenobarbital. You cannot start giving them on your own.
For epilepsy, tetanus or intoxication, hospital treatment is indicated. Drugs aimed at eliminating seizures and vitamins are administered.
Urgent hospitalization is also required for newborns. The baby will be closely monitored in the intensive care unit.
Even if the convulsive episode recurs only once, children are registered and observed for 12 months.
Consequences
The occurrence of convulsive syndrome in newborns, especially premature ones, can lead to death. It is noted that with unknown causes of repeated attacks, such children develop encephalopathy or ischemic stroke. Death is often possible with meningococcal infection.
Seizures due to metabolic disorders and febrile seizures are usually treatable. The latter pass without leaving a trace, especially in infants. But if attacks occur in older children and appear repeatedly, then there is a risk of oxygen starvation, mental retardation and severe damage to all areas of the personality.
It is important to remember that the onset of an attack is accompanied by impaired coordination of movements and loss of consciousness. If you fall on asphalt, hard surfaces, or sharp objects, you can get injured, including traumatic brain injury. First aid should include safety measures for the victim.
It is better not to leave children prone to epilepsy alone at night. During the night's rest, when no one is watching the child, it is possible to fall out of bed, get pinched and bite off the tongue.
Symptoms of epilepsy
The manifestations of epilepsy attacks may differ from patient to patient. First of all, the symptoms depend on those areas of the brain where the pathological discharge occurs and spreads. In this case, the symptoms will be directly related to the functions of the affected parts of the brain. Movement disorders, speech disorders, an increase or decrease in muscle tone, and dysfunction of mental processes can occur, both in isolation and in various combinations.
The severity and set of symptoms will also depend on the specific type of epilepsy.
Jacksonian attacks
Thus, during Jacksonian attacks, pathological irritation covers a certain area of the brain without spreading to neighboring ones, and therefore the manifestations concern strictly defined muscle groups. Typically, psychomotor disorders are short-lived, the person is conscious, but it is characterized by confusion and loss of contact with others. The patient is not aware of the dysfunction and rejects attempts to help. After a few minutes the condition is completely normalized.
The twitching or numbness starts in the hand, foot, or leg, but can spread to the entire side of the body or develop into a grand mal seizure. In the latter case, they speak of a secondary generalized attack.
A grand mal seizure consists of successively alternating phases:
- Precursors - several hours before the onset of an attack, the patient is seized by an anxious state, characterized by an increase in nervous excitement. The focus of pathological activity in the brain gradually grows, covering more and more new sections;
- Tonic convulsions - all muscles tense sharply, the head is thrown back, the patient falls, hitting the floor, his body is arched and held in this position. Due to respiratory arrest, the face turns blue. The phase is short, about 30 seconds, rarely up to a minute;
- Clonic convulsions - all the muscles of the body contract rapidly rhythmically. Increased salivation, which looks like foam at the mouth. Duration – up to 5 minutes, after which breathing is gradually restored, the cyanosis disappears from the face;
- Stupor - in the focus of pathological electrical activity, strong inhibition begins, all the patient’s muscles relax, and involuntary passage of urine and feces is possible. The patient loses consciousness and there are no reflexes. The phase lasts up to 30 minutes;
- Dream.
After waking up, the patient may suffer from headaches, weakness, and movement disorders for another 2-3 days.
Minor attacks
Minor attacks are less pronounced. A series of twitching of facial muscles, a sharp drop in muscle tone (as a result of which a person falls) or, conversely, tension of all muscles when the patient freezes in a certain position may occur. Consciousness is preserved. There may be a temporary “absence” – absence. The patient freezes for a few seconds and may roll his eyes. After the attack, he does not remember what happened. Minor seizures often begin in preschool age.
Status epilepticus
Status epilepticus is a series of seizures following each other. During the intervals between them, the patient does not regain consciousness, has reduced muscle tone and lack of reflexes. His pupils may be dilated, constricted, or of different sizes, and his pulse may be rapid or difficult to feel. This condition requires immediate medical attention, as it is characterized by increasing brain hypoxia and swelling. Lack of timely medical intervention leads to irreversible consequences and death.
All epileptic seizures have a sudden onset and end spontaneously.
Symptoms of the disease
The main symptom of the pathology, by which epilepsy can be accurately identified, is a seizure. In adolescence, they differ in the following points:
- there is a feeling of a sharp blow in the area under the knee, which causes the need to sit down, in some cases the child falls to the ground;
- symmetrical convulsions appear, during which a person bends and straightens his arms and legs;
- sharp muscle contractions cause a person to drop or involuntarily throw objects.
Indirect signs of pathology can be identified, which are often detected at the age of 10-11 years. Many of the symptoms are related to sleep: sleepwalking, screaming during sleep, nightmares.
The child suffers from headaches that occur frequently and out of nowhere, often accompanied by bouts of vomiting. Speech is impaired in adolescents. Aggression gradually appears. After diagnosis, a person becomes withdrawn and tends to ignore medical and parental recommendations.
Localization of the focus of epilepsy: focal seizures
Focal seizures begin from a specific point and do not involve the entire cortex. Depending on the place where the pathology begins, the symptoms differ:
Develops in most cases of focal seizures. Affects the emotions, memory and feelings of a teenager. Symptoms such as sudden changes in mood and strange thoughts or emotions appear. The child becomes anxious and does not understand what is happening.
- Frontal epilepsy
Symptoms of seizures depend on the area of the frontal lobe that is involved in the pathology. Sudden convulsions occur and pass quickly enough. There is marked weakness in the muscles, including those responsible for speech. Often attacks begin in a dream: the child rushes about uncontrollably, turns his head, moves his legs. Due to the large size of the frontal lobe, sometimes symptoms cannot be identified (they are believed to be hidden).
- Parietal epilepsy
Most of the symptoms affect human sensory receptors. In a teenager, epilepsy manifests itself as mixed sensations in different areas of the body: sudden warmth, tingling, an imaginary change in body size, partial numbness.
The least common form of adolescent epilepsy, which may cause changes in vision. The child experiences flashes of colors before the eyes, black dots, patterns, or images. Also with this form there is a flickering sensation, which causes a feeling of nausea.
Some children experience partial blindness at the time of the attack, uncontrolled eye movement, and painful sensations on the eyelids. When the attack lasts for a long time, severe headaches develop.
There is a second form of attacks, which are extensive and manifest with severe symptoms.
Generalized seizures
Generalized seizures are so called because in epilepsy all parts of the brain are affected by the improper action of neurons. In 100% of cases, the person loses consciousness or is in a semi-fainting state, cannot think soberly and cannot stand on his feet.
Sometimes epileptic seizures begin as focal ones, but can develop into generalized ones. They can be identified by special beacons indicating loss of consciousness. To avoid injury, a person must sit comfortably. Types of seizures:
- Tonic-clonic. It begins with an acute phase, accompanied by a cry due to spasms of the vocal muscles responsible for contracting the gap. Air escapes from the larynx, and convulsions of the limbs occur. They run out in a few minutes. The person may experience severe drowsiness and confusion. Almost always, a teenager needs rest after an attack. If a seizure lasts longer than 5 minutes, emergency medical assistance is needed.
Types of attacks and accompanying symptoms
There are three types of myoclonus epilepsy attacks:
- Myoclonic. Characterized by muscle twitching that cannot be controlled. They usually occur in the morning, but can also be triggered by fatigue, strong emotions, alcohol consumption, sound or light exposure. The presence of cramps can be observed both in an individual muscle or limb, and throughout the body.
- Absence seizures. Consciousness turns off suddenly for a short period of time. It is caused by a lesion in the brain that affects its different parts. In this state, a person is in a stupor for several seconds, while his gaze also freezes, speech and movement stop. Despite their short duration, absence seizures lead to serious disturbances of consciousness.
- Tonic-clonic. The whole body is subjected to a convulsive state. In addition, loss of consciousness is observed. Involuntary urination or defecation is possible. The duration of the attack is several minutes. They are observed in more than half of patients and usually occur during awakening.
Everything you need to know about sleep epilepsy
- Polina Yurievna Timofeeva
- March 26, 2020
Myoclonic epilepsy is classified into several forms:
- Infants are benign in nature. This is a rare type of disease. Its development can last from several months to five years. However, it has not yet been possible to determine the root cause. The only thing is that in rare cases it can transform into an adolescent form, practically does not cause serious complications and quickly passes with correct and timely treatment. May be accompanied by twitching of the limbs or head, and sometimes the body. Myoclonus may also vary in intensity. During the period when a person falls asleep, they intensify, and during sleep they disappear. In this case, psychomotor development is not damaged in any way. The diagnosis is made based on the collection of anamnestic data.
- Dravet syndrome is severe and occurs in 5 percent of infants. Until the symptoms begin to manifest themselves, the child develops normally. This type of attack often provokes severe psychoneurological disorders, sometimes even fatal.
- Unferricht-Lundborg disease. It is considered the more common form. Observed during late childhood. The pathology begins to manifest itself with myoclonus, which is subsequently complicated by absence seizures and focal attacks. The disease develops slowly. Over the course of many years, the patient’s intellectual abilities remain unchanged, but afterward there is a decrease in memory and frequent depressive states. The disease has periods of remission and exacerbation, which leads to the fact that the patient is forced to spend all his time in bed. The diagnosis is based on the clinical picture. With timely treatment, there is a chance of slowing the development of pathology, which allows the patient to live to old age.
- Myoclonic epilepsy with broken fibers. This form provokes the development of abnormal DNA. In most cases it is observed in childhood and adolescence, but it also occurs in adults. In addition to the fact that this form is accompanied by tonic convulsions and myoclonus, the patient’s coordination is impaired, deafness and myopathy progress. During diagnosis, torn fibers can be seen in the skeletal muscles, and the content of lactic acid in the blood increases significantly.
Conventionally, the course of the disease can be divided into three stages:
- Epileptic-titaniform - can last for several years. As the disease progresses, attacks become more frequent, accompanied by painful spasms and increased sweating. The patient is conscious. As a rule, at this stage there are no neurological disorders, but the patient may exhibit aggression, depression or withdrawal.
- Myoclonic-epileptic – often can last for many years. The number of seizures decreases, and attacks of myoclonus occur. At the beginning, muscle contractions occur only in part of the limb, gradually spreading to the entire body. The patient loses the ability to eat and write independently. While walking, there is a bending from side to side.
- Terminal – leads to serious changes at the mental level, which is expressed by memory and speech disorders.
It should be noted that the last stage can lead to dementia of the patient.
Main signs of the disease
In order to choose the right strategy for correcting the disease, you need to find out its etiology. Doctors distinguish several causes of epilepsy in children:
- Heredity. Scientists have identified a substance—dopamine—that is responsible for inhibiting overexcited neurons. Its volume is programmed in the genes: if parents have epileptic seizures, then there is a chance that their offspring will inherit them.
- Malformations of the fetal brain. The health of the future person in the womb is influenced by everything: at what age she conceived (middle-aged first-born women are included in the risk group), what illness she had, how she was treated, whether she abused drugs or alcohol. Poisoning of the embryo with toxic substances is the main cause of brain pathologies.
- Birth injuries. The causes of epilepsy often lie in the excesses that accompany the birth process. The baby's brain can be damaged by the midwife's forceps, prolonged labor, or squeezing the newborn's neck with the umbilical cord.
- Inflammatory diseases of the brain and its membranes: encephalitis, meningitis, arachnoiditis.
- Febrile convulsions during colds can reveal epilepsy in children with a family history.
- Traumatic brain injuries. Mechanical blows to the head often lead to the appearance of epileptogenic foci in the brain.
- Volumetric neoplasms. Tumors pressing on the brain can cause seizures in children.
- Metabolic disorders manifested by hyponatremia, hypocalcemia, hypoglycemia.
- Cerebral blood flow disorders.
- Teenagers' addiction to ephedrine, amphetamines and other drugs.
Symptoms of epilepsy in children are sometimes mistaken by hapless adults for excessive physical activity. This is the main reason for the late detection of a dangerous disease. Another common mistake is to think that an epileptic seizure can only involve convulsions and foaming at the mouth.
In order not to waste precious time, parents of children need to have a detailed understanding of the clinical picture by which childhood epilepsy is recognized.
Its features are quite diverse:
- Generalized convulsive seizures. They begin with an alarming harbinger - an aura. At this stage, the patient feels something like a breath running through the body or other unusual sensations. Then comes the stage of sharp muscle tension and holding the breath - the child falls screaming. The turn of convulsions comes, the eyes roll back, foam appears at the mouth, spontaneous urination and bowel movements may occur. Convulsive twitching can affect the entire body or muscle group. The attack lasts a maximum of 20 minutes. When the convulsions stop, the patient comes to his senses for a few moments and immediately falls asleep, exhausted.
- Nonconvulsive (minor) seizures. These not always noticeable attacks of epilepsy in children are called absence seizures. It all starts with the baby suddenly freezing with a blank look. It happens that the patient’s eyes are closed and his head is thrown back. For 15-20 seconds he does not perceive anything. Having emerged from a painful stupor, he returns to the interrupted business. From the outside, such pauses may seem thoughtful or absent-minded.
- Atonic seizures. The manifestation of attacks of this kind consists of a sudden loss of consciousness and muscle relaxation. They are often mistaken for fainting. The frequency of such conditions should be alarming.
- Baby spasm. Epilepsy in a baby can be manifested by a sharp raising of the arms to the chest, an involuntary tilt of the head and body forward when straightening the legs. This happens most often with children 2-4 years old when waking up in the morning. The attack lasts for several seconds. By the age of 5, the alarming manifestations of the disease either disappear or take a different form.
- Speech disturbance for several minutes while maintaining consciousness and the ability to move.
- Frequent nightmares, causing the baby to wake up screaming and crying.
- Sleepwalking.
- Regular headaches, sometimes causing nausea and vomiting.
- Sensory hallucinations: visual, olfactory, auditory, gustatory.
The last four signs do not necessarily indicate epilepsy. If such phenomena begin and begin to recur repeatedly, parents need to conduct a psychoneurological examination of the child.
Juvenile or juvenile myoclonic epilepsy is a special benign form of idiopathic generalized epilepsy, which manifests itself in the form of myoclonic seizures in children and adolescents. The peculiarity of myoclonic seizures is that they most often occur upon awakening. Massive bilateral myoclonic seizures often occur, that is, seizures involving paired organs (limbs, eyes).
The first description of this type of disease dates back to 1867, but juvenile epilepsy became a separate disease in 1955 at the suggestion of German doctors led by Dr. Janz. Because of this, this form of epilepsy is sometimes called Janz syndrome.
The disease begins in childhood or adolescence. This type is considered quite common, since 8-10% of all epileptics suffer from this form of the disease.
- Juvenile epilepsy is equally common among both men and women.
- The psychological status of patients is most often normal; the disease does not in any way affect the mental development of the patient.
- The disease is diagnosed fairly quickly, responds well to treatment, and the patient can be observed by an epileptologist for the rest of his life for preventive purposes.
The onset of the disease ranges from 8 to 24 years, with the peak occurring between 10 and 14 years. Sometimes there were cases when the disease was diagnosed in children under 1 year of age.
The main symptoms of the disease are seizures, which are of three types:
- Myoclonic seizures. Spontaneous twitching of the facial and limb muscles. Myoclonus usually occurs in the first few hours after waking up. With severe overwork, cramps begin even before bedtime. During convulsions and twitching, the patient cannot hold anything in his hands and becomes clumsy and awkward. Sometimes such cramps interfere with everyday activities: eating, doing homework, tidying up. If myoclonic seizures are the only symptom, they often go undiagnosed because they are perceived as tremors or nervousness.
- Tonic-clonic seizures. Seizures that occur approximately three hours after waking up from sleep. They occur in half of patients with Janz syndrome. The attacks are accompanied by more severe convulsions than during a myoclonic seizure; often when they occur, the patient screams or wheezes. Most often, loss of consciousness occurs as spasms of the chest muscles make breathing difficult.
- Absence seizures. Short-term attacks lasting 10-40 seconds, which are characterized by loss of consciousness. Absence seizures are not accompanied by convulsions and can occur at any time of the day. They can be either the first symptoms of Janz syndrome or appear in the later stages of the disease.
Many children and adolescents with juvenile epilepsy have photosensitivity. Patients with this phenomenon are especially sensitive to bright flashes of light, which can trigger a seizure. Such patients need to limit watching television, spending time at the computer, visiting cinemas and discos, especially during the period when the disease worsens.
Symptoms such as perioral reflex myoclonus also occur among patients. These are small twitches in the muscles of the tongue, lips or larynx that occur while reading or talking.
Some epileptics experience sensitivity when closing their eyes. These are mild bursts of brain activity lasting about 2-3 seconds, which are observed when blinking the eyes on the electroencephalogram.
Most often, the symptoms of the disease are not a single type of attack, but a combination of them. Many people recognize the disease when tonic-clonic seizures already appear.
Patients should be carefully questioned about all possible symptoms to avoid missing myoclonic seizures, which are an important feature of Janz syndrome.
Patients do not always pay attention to small twitching of the lips and fingers, believing that this has nothing to do with epilepsy.
Not long ago, Japanese scientists discovered that juvenile myoclonic epilepsy is associated with a phenomenon called “praxis induction.” This is a phenomenon that is characterized by the occurrence of an attack while performing difficult tasks associated with the involvement of mental and mental activity. For example, when playing computer games, doing complex calculations or playing chess, myoclonic twitching may begin.
Most often, attacks are triggered by interrupted sleep. After waking up or during breakfast, an attack occurs.
Sometimes seizures are caused by drinking alcohol. Alcohol has a negative effect on the nervous system, which instantly disrupts brain function.
An important provoking factor is overwork. This can be overwork, both physical and mental. Sometimes parents, trying to protect their children from overwork, limit their mobility. But this factor can also negatively affect the likelihood of a seizure.
Lack of sleep and insomnia can provoke seizures.
Juvenile myoclonic epilepsy most often occurs due to a hereditary factor. If parents or immediate relatives of children and adolescents suffered from epilepsy, there is a high chance of Janz syndrome. There are several reasons that contribute to the occurrence of juvenile epilepsy:
- tumors and neoplasms in the brain;
- acquired traumatic brain injuries;
- head injuries acquired during pregnancy or while the baby was passing through
- birth canal;
- infectious diseases;
- impaired cerebral circulation.
Sometimes children with absence epilepsy later develop juvenile epilepsy.
Most geneticists are inclined to believe that juvenile myoclonic epilepsy is a genetic disease, that is, its occurrence is based on defects in certain genes.
Signs and symptoms
Disease prevention
Once diagnosed with juvenile myoclonic epilepsy, treatment with medications alone may not be enough. With this disease, it is necessary to follow a certain daily routine, especially with regard to sleep: you should not go to bed too late, you should get up every day at the same time. It is imperative to exclude factors of photostimulation in everyday life. As far as possible, you should avoid any alcoholic beverages and not drink them even in small quantities. Proper nutrition matters. If you follow a daily routine and avoid unfavorable factors, the disease will be much easier to bear.
Prevention of juvenile myoclonic epilepsy consists of actions that prevent the development of epileptic seizures in the patient.
To do this, it is recommended to carry out the following activities:
- Timely diagnosis of hereditary diseases and chromosomal syndromes.
- Identification during examination during pregnancy of women who have an increased risk of giving birth to a child with Janz syndrome. As a rule, these are women suffering from various endocrine diseases, drug addicts, and so on.
- Monitoring children born with low body weight and other abnormalities, as well as developing a strategy for their treatment.
- Performing social activities for patients with juvenile myoclonic epilepsy.
Janz syndrome is a fairly common phenomenon in medicine, it has been well studied, so specialists can help almost all patients who are faced with this problem to completely get rid of it. Most people with this diagnosis can lead quite active and fulfilling lives.
Myoclonic spasms in children
Mild myoclonic spasms in children, as in adults, often occur during sleep and when falling asleep. In these cases, the child may even wake up and get scared. In infancy, tight swaddling will help prevent this. As an adult, you can cover the child with a heavy blanket or tuck its edges under the mattress.
In some cases, myoclonic twitching in children is one of the signs of the development of epilepsy. It can be congenital, or hereditary, or acquired. Many factors can cause this pathology. Boys are more prone to its development.
There is an age-related benign form of idiopathic epilepsy called juvenile myoclonic epilepsy or Janz syndrome. This disease occurs in adolescents during puberty and goes away over time. Various factors can trigger an attack of convulsions: bright light, fear, severe stress, a loud sharp sound, etc.
Symptomatic epilepsy in children: treatment of the cause and treatment of symptoms
The causes of epilepsy are not fully understood. Moreover, there are many more unexplored facts regarding this disease than reliably known ones. This statement does not apply only to symptomatic epilepsy - epilepsy that arises from any known, “material” factor.
What can cause symptomatic epilepsy? Almost any condition, without exaggeration. Brain abscess, hematomas, hemorrhages, injuries, inflammatory diseases or metabolic disorders - all this can cause the development of epilepsy in a child.
Actually, that’s all the difference between this form and “ordinary” epilepsy: its cause can be identified, and, therefore, can be eliminated. The main postulate of the treatment of symptomatic epilepsy: you need to act on what caused the disease, and not just on its symptoms.
Diagnostics
The initial clinical examination is indicative only. To make a correct diagnosis, additional laboratory and instrumental examinations are required.
Today, electroencephalography (EEG) is considered the “gold standard” for diagnosing this disease. It should be noted that every second child does not experience any changes in the electroencephalogram during the period of absence of an attack.
Identifying specific signs directly during a seizure attack allows you to accurately make a correct diagnosis. In complex clinical situations, when diagnosis is very difficult, several EEGs or daily monitoring of this indicator are required.
Such a study not only allows you to clarify the correct diagnosis, but also determine the prognosis and further treatment tactics. The studies included in neuroimaging include computed tomography and magnetic resonance imaging. MRI allows you to clarify local areas of pathological tissue, which trigger the appearance of unfavorable characteristic symptoms in the baby.
Children with epilepsy undergo multiple laboratory tests. These include general clinical blood and urine tests, biochemical blood tests, determination of specific autoantibodies and glucose and lactate levels, as well as serological tests.
In some cases, the examination plan also includes an ultrasound examination of the abdominal organs, Dopplerography of the vessels of the neck and brain, electrocardiography and other studies.
My leg cramped! How to help a child with muscle cramps?
Contrary to popular belief, hardening does not require low temperatures.
It requires temperature contrast. Cold causes blood vessels to constrict; heat causes them to expand. And the main thing in hardening is vascular training. Pediatricians regularly encounter complaints of leg cramps, both from teenagers and very young children. Most often, cramps occur while falling asleep or in the middle of the night, causing the child to wake up with sharp pain. Why does such an unpleasant phenomenon occur and how to deal with it? A cramp is an involuntary contraction of one or more muscle groups, in other words, a spasm. When a leg cramp occurs, the calf muscle, located on the back of the lower leg, usually cramps. The spasm can be so strong that the child is simply unable to straighten his foot, and from the outside it seems as if he is standing on his tiptoes.
There are actually many possible reasons for the occurrence of such seizures. But there are three main factors that lead to the vast majority of calf cramps in children.
First of all, this is an imbalance of vitamins and microelements, especially a lack of magnesium.
More than half of the cramps in the lower extremities are associated with a deficiency of this mineral, as it is necessary to relax the muscles and relieve hypertonicity.
A lack of potassium and calcium can also affect it. Leg cramps often plague children during a period of active growth, when many vitamins and minerals are consumed by the child’s body at an accelerated pace.
Long-term, excessively intense stress on the legs, such as running, swimming, football, etc., also leads to cramps. Children, compared to adults, are very active physically.
They have the amazing ability to not feel tired when they are overwhelmed by something. For example, a preschool child can ride a bicycle for hours until completely exhausted without realizing it.
In this case, night cramps become the body’s reaction to overload.
In addition, spasms of the calf muscles can be a harbinger of incipient or already developed flat feet.
The listed reasons are most likely if the child has been experiencing regular seizures for a long time. But there are also reasons for “one-time” spasms of the calf muscles:
- Finding the leg in an awkward position and in an unchanging position;
- Hypothermia of the lower extremities (swimming in a body of water at low water temperatures is especially dangerous).
Prolonged and intense stress on the legs causes spasms in the calf muscles.
First aid for leg cramps
When a child's leg cramps, you need to perform an action that will stretch the calf muscle. This is the basic principle of first aid for cramps. The child should pull the toe of the flattened leg towards himself, as if straightening it.
This may cause sharp pain for a few seconds, but then the cramp should subside. If the condition does not improve, you should weaken the cravings and then strengthen them again.
But if this procedure does not help, you need to get up and walk around a little to speed up the blood flow in the limb and help relieve the spasm.
Then you need to massage the muscle and apply a heating pad or simply put your leg in a bath with warm water.
After this, ask the child to lie down for ten minutes with his legs elevated - this will improve the flow of blood in the extremities and reduce the likelihood of a recurrent cramp.
If you have a leg cramp, you need to stretch the calf muscle.
Treatment and prevention of seizures
A child experiencing regular seizures should visit a pediatrician. The attending physician will prescribe an examination and, if necessary, give a referral to more specialized specialists, for example, to an orthopedist in case of suspected flat feet.
Parents should adjust the baby’s diet by adding foods rich in magnesium and potassium to the diet. These include legumes, carrots, green leafy vegetables, seaweed, bananas and dried apricots.
Taking children's vitamin and mineral complexes will also be useful.
Organize the child's sleeping area so that the child sleeps with his legs slightly elevated. To do this, you can place several sofa pillows or a bolster on the edge of the bed. Before going to bed, your baby can have a light foot massage with warming ointment (this should be chosen on the advice of a pediatrician) or take a warm bath.
Of course, if a child experiences great physical stress on his legs while playing sports, the intensity of training will have to be reduced for some time. In general, cramps will not bother the baby for long when family members notice and promptly begin to solve this problem.
Source: https://schoolofcare.ru/articles/nogu-svelo-kak-pomoch-rebenku-pri-mishechnikh-sudorogakh/
Epilepsy remission
What is complete remission of epilepsy?
Complete remission -
This is the complete suppression of all seizures and epiactivity on the EEG, in the absence of pronounced side effects from the treatment used, while maintaining a high quality of life.
What time period is sufficient to say that remission of epilepsy has occurred?
It is generally accepted that remission is the complete absence of attacks for 12 months.
How to achieve remission from epilepsy?
Use antiepileptic drugs for treatment.
We begin therapy immediately after diagnosis and clarification of the form of epilepsy according to the classification.
First, we use one antiepileptic drug in treatment, selecting the dose depending on the effectiveness and safety. If ineffective, we introduce a second drug. Further polytherapy is possible. The process of selecting therapy is complex and individual, but is based on clearly developed principles of therapy.
In a small number of people, surgical treatment may be used. An option for treating drug-resistant forms of epilepsy in addition to taking medications is a ketogenic diet or stimulation of the vagal nerve.
In cases where it is not possible to achieve complete electro-clinical remission, we achieve the maximum possible improvement in the patients' condition. This is how the terms are distinguished:
1. Incomplete remission
,
when the patient has no seizures, but epiactivity on the EEG remains and there are changes in intellectual-mnestic functions (the term
“remission of epileptic seizures”
).
2. P pseudoremission
-
those cases when, while taking anticonvulsants, the patient himself and those around him do not notice any seizures; but when carrying out the necessary diagnostics (most often, video EEG monitoring, when seizures and synchronous epiactivity are clearly recorded on the EEG).
What do we call recovery from epilepsy?
Complete electro-clinical remission for 5 years while taking AEDs and another 5 years without treatment, the absence of progressive changes in the mental sphere, can be called recovery
.
Epilepsy remission
Based on the materials of the conference on epilepsy in Krasnoyarsk, held in February 2014, where, together with major scientific figures in epileptology, such important concepts as “remission”, “pseudo-remission” and others were proposed. These and other terms should be generally accepted so that all doctors - neurologists, epileptologists, as well as doctors of other specialties and, of course, patients with epilepsy understand each other. These are important stages in the development of epileptology that determine the treatment tactics for each patient. How to treat epilepsy, how long to treat epilepsy, how often and for a long time to monitor the patient after the seizures have stopped? It is these questions that the adopted terminology answers. This is the first article on remission; further we will examine the terms “remission failure”, “pharmaco-resistance” and others.
Preparing for diagnosis: what parents should remember
If epilepsy is suspected in a teenager, parents can prepare for the diagnosis so that it is more effective:
- you need to tell the neurologist when the seizures started,
- describe the seizures in detail: position of the arms, legs, body and head, condition of the pupils and skin color, duration,
- the specifics of the course of the attack - sharply or with an aura (preceding sensations),
- time of occurrence of the first seizures,
- what are the provoking factors: stress, temperature, menstrual cycle in girls, working at the computer,
- the child's behavior before the seizure.
After visiting a neurologist, they will prescribe electroencephalography of the brain, MRI and CT, as well as mandatory blood, stool and urine tests. Sometimes a cerebrospinal fluid test is needed to rule out other diseases.
Signs and symptoms
Myoclonic seizures indicate the occurrence of juvenile epilepsy.
They do not last long and are involuntary asynchronous muscle contractions. Most often, seizures occur in the morning, after waking up.
Muscle contractions usually involve only the arms and shoulder girdle, but in some cases they spread to the legs or even the entire body.
During an attack, patients may drop or throw away objects they were holding in their hands. If the lower extremities are involved in a seizure, adolescents fall.
Rarely, patients present with myoclonic status epilepticus. The patient does not lose consciousness. In 3-5% of cases, the disease occurs with only myoclonic seizures.
3 years after the first attack, in the vast majority of cases, tonic-clonic seizures develop.
They begin with increasing myoclonic twitching, which turns into clonic-tonic convulsions. 40% of such patients experience absence seizures. They lose consciousness for a short period.
Cramps in the hands
The causes of hand cramps are very numerous and varied. Any cramps, including those in the hands, are involuntary muscle contractions. A person cannot control them, but he can provide himself with first aid, which does not require special skills.
Why do my hands cramp? There are many reasons for this problem, but they are all a consequence of a person’s incorrect attitude towards his body. Quite often, finger cramps bother those who work a lot at the computer. Their hands are tense and remain in the same position for a long time, making the same type of movements. The result of such work is chronic “numbness” of the fingers and hands.
Only a doctor can find out the cause of seizures after receiving the results of a complete examination of the person. When choosing therapeutic measures and medications, it is necessary to take into account the patient’s age, his general condition, life history and illness, the presence of concomitant pathologies and diseases that he has suffered.
We suggest that you familiarize yourself with Treatment of testicular varicose veins with folk remedies
The causes and treatment of hand cramps are in a close interdependent relationship: once the specific cause of this pathology is identified, it is easy to select a treatment that will give the expected result in the shortest possible time. In general, stopping an attack of cramps in the hands is quite simple, regardless of the time of day at which it began: at night, during the day, at the height of working hours.
If there are no results from self-treatment, you can seek help from a reflexologist. Sometimes the cause of spasms in the arm muscles is the regular impact on active points of the body, which causes increased blood flow in the tissues and leads to the formation of cramps. Only a specialist will be able to determine such a cause and find the optimal method to get rid of seizures forever.
Causes and manifestations of pathology
It is not known exactly why nocturnal epilepsy occurs. But the main factor contributing to the occurrence of convulsive seizures is considered to be the lack of proper sleep.
Frequent lack of sleep leads to depletion of the energy reserves of the central nervous system, disruption of the processes of excitation and inhibition. As a result, epileptogenic foci are formed in the cerebral cortex. The longer a person neglects rest, the higher the likelihood of seizures occurring during sleep.
Possible causes of epilepsy at night also include:
- physical, mental stress;
- regular use of alcohol, drugs;
- frequent stress;
- suffered traumatic brain injuries;
- infectious diseases;
- congenital abnormalities of brain development;
- genetic predisposition;
- injuries during childbirth;
- neoplasms in the brain.
It is impossible to independently understand what triggered the occurrence of convulsive seizures during sleep. Only a doctor can determine the cause of the development of epilepsy and select the correct treatment after the patient has undergone an examination.
In the nocturnal form of epilepsy, seizures most often occur in the first half of the night, during the REM sleep phase (this is due to changes in brain activity). Their appearance can be triggered by a sudden awakening or a sudden phone call.
If the disease progresses, convulsive crises appear in any phase of sleep, regardless of the presence of provoking factors. Let's look at the main types of attacks (Table 1).
Table 1 - Types of nocturnal seizures
| Early night | Occurs 2 hours after the patient falls asleep |
| Morning | Starts in the morning, an hour before or after waking up |
| Mixed | Cramps occur during night and day rest |
The symptoms of nocturnal epilepsy are practically no different from the clinical picture of the daytime form of the disease. Immediately before a seizure appears:
- intense headache;
- feeling of discomfort;
- nausea;
- spasm of the facial and laryngeal muscles;
- speech disorder;
- chills.
Differential diagnosis of seizures
After these symptoms appear, cramps occur in a specific muscle group. They then spread in a sequence corresponding to the location of the brain centers that control movement. The patient has difficulty breathing and increased salivation. Involuntary urination and defecation may occur.
Clinical manifestations of epilepsy at night in adults can be supplemented by symptoms that are characteristic of a sleep disorder:
- sleepwalking;
- nightmares;
- panic attacks;
- walking and talking while sleeping.
In general, an epileptic seizure lasts from 10 seconds to 5 minutes. After this time, the person falls asleep. After waking up, he does not remember the events that took place during the night. Epilepsy during sleep is not always accompanied by seizures. Non-convulsive seizures can be recognized by the following signs:
- dilated pupils;
- blank look;
- lack of response to the environment.
WHAT IS EPILEPSY
Epilepsy (the ancient Greek word “Epylepsis”) translated means something like “to collect, accumulate.” Epilepsy is a disease known since ancient times. For a long time, there was a mystical idea of epilepsy among people. In ancient Greece, epilepsy was associated with witchcraft and magic and was called a “sacred disease.” It was believed that epilepsy was associated with the possession of spirits and the devil in the body. God sent it to a person as punishment for an unrighteous life.
Mention of epilepsy is also found in the Gospel of St. Mark and from St. Luke, where Christ’s healing of a boy from the devil who had entered his body is described. In the Middle Ages, attitudes towards epilepsy were ambivalent. On the one hand, epilepsy caused fear as a disease that could not be cured, on the other hand, it was often associated with obsession and trances observed among saints and prophets. Christian theologians noted that certain passages of the Koran indicate that Mohammed suffered from epilepsy. His attacks were accompanied by drooping of the eyeballs, convulsive movements of the lips, sweating, snoring, and lack of reaction to the environment. It is assumed that St. also suffered from epilepsy. John and St. Valentin.
Complications, prognosis and prevention
The prognosis for treating the disease is moderately favorable if therapy is started in a timely manner. In such cases, it is possible to almost completely eliminate symptoms and seizures to the level of local nervous tics.
Formally, we can say that in this case epilepsy is cured, but if therapy is carried out late or the wrong drugs are prescribed, the average life expectancy of the patient is about 20 years (although some live to a ripe old age even with severe seizures).
In such cases, complications of epilepsy lead to death: pneumonia, cachexia and other associated pathologies.
Infant forms of pathology are fraught with mental disorders and retardation of children in intellectual development.
There are no special effective preventive recommendations that would allow one to avoid the development of the disease, but the risk of this can be reduced if, in childhood, one limits the consumption of caffeine-containing products and eats more fruits and vegetables that are rich in plant fiber.
Myoclonic seizures sometimes occur in healthy people. They are often observed during serious physical activity (this can often be seen in athletes), but if this happens in adults, there is generally no reason for concern.
But if signs such as twitching of the eyes, facial muscles and hands are observed in childhood and without obvious prerequisites, the child should be shown to a doctor.
Perhaps this will make it possible to recognize the disease in time and begin treatment, thanks to which pathological complications will be kept to a minimum.
About errors in the treatment of myoclonic epilepsy in this video:
Features in teenagers
The disease occurs in childhood, and most cases occur in adolescence. In rare circumstances, hereditary epilepsy due to concomitant causes manifests itself at the age of 20 years. The first seizures begin at 11–16 years of age, but in rare cases they occur for the first time only at 17–19 years of age.
Thus, children's “falling sickness” is often not accompanied by deep fainting or convulsions. The attacks go unnoticed, or are more like a nervous breakdown. Even at a young age - up to 11 years - parents are practically unable to notice this pathology. At school, the disease begins to make itself felt: it is difficult for the child to concentrate, and he begins to lag behind in his studies.
Absence in children
Absence seizures in children first appear at the age of 2-4 years, when the formation of brain activity is completed. However, attacks may occur later. Absence seizures in children can be easily corrected with timely therapeutic intervention. Complete recovery in such cases is observed in 70-80% of patients.
In children, epilepsy attacks occur suddenly. Sometimes it is possible to identify an incipient seizure by the following phenomena that worry the child against the background of general health:
- headache;
- increased sweating;
- active heartbeat;
- panic mood;
- aggressive behavior;
- sound, taste, auditory hallucinations.
In children, the duration of epilepsy attacks is usually 2-30 seconds. Less common are myoclonic absence seizures, in which the muscles of the arms, legs, face, or entire body cramp. Movements can be unilateral or asymmetrical. A combination of eyelid myoclonus and absence seizures is very rare. Most attacks are caused by uncontrollable twitching of the muscles in the mouth area.
Forms of the disease
There are different forms of epilepsy in adolescents, but they are all different from adult types.
| Type of disease | Peculiarities |
| Juvenile absence epilepsy | It is characterized by generalized muscle contractions, gradually turning into absence seizures. As the temperature rises, febrile seizures begin |
| Juvenile myoclonic form (constant relapses and development due to insomnia, forced awakening, alcohol intake) | The disease begins with small muscle twitching in the shoulder girdle, after some time generalized convulsions develop, and the frequency of attacks can reach 1 time per day |
| Form with generalized seizures | Seizures may appear once a year, but there are cases when the disease occurs every week |
| Catamenial epilepsy (occurs in girls) | Seizures depend on the phase of the menstrual cycle |
The severity of the symptoms of epilepsy in a child, as well as treatment methods, depend on the type of disease.
Forms of attacks
Conventionally, the forms of myoclonus have acquired the names benign and negative. Benign myoclonus does not require treatment. As a rule, they are observed at night or when a person falls asleep. The duration of the attacks is short - up to several minutes. In a conscious state, fear myoclonus occurs. Spasmodic conditions are provoked by a sharp cry, the fall of any object, or bright flashes of light. The condition is accompanied by tachycardia and sweating. As a result of an attack, hiccups sometimes occur. Involuntary hiccups also indicate chronic diseases of the gastrointestinal tract and intoxication of the body.
Paroxysmal numbness of the calf muscles and eye tics indicate physical overexertion. Such benign myoclonus is typical for children in the first months of life, observed during sleep, and during lactation. Myoclonus cannot be ruled out when the child falls asleep. It is possible to observe involuntary contractions of the neck muscles, limbs and back. As a rule, symptoms disappear within a year without special correction.
Negative myoclonus refers to epileptic seizures. A clear example of the mentioned attacks in children and adults is a slight tremor of the arms when in an extended position. An attack occurs in any type of muscle tissue, even the tongue.
Tonic-clonic seizures
A tonic-clonic seizure is the first thing people think of when they hear the word “epilepsy.”
The attack begins with a tonic phase, which is characterized by a peculiar cry (convulsions of the muscles of the glottis), during which air escapes from the larynx. The clonic phase is characterized by convulsive twitching of the limbs, which subside and ends, usually within a few minutes.
After an attack, a person may experience drowsiness, confusion, and agitation, so he needs rest and sleep.
If a tonic-clonic seizure lasts more than 5 minutes, emergency medical attention is needed.1
The question of how to recognize epilepsy in a child under one year old is extremely important. In infancy, the disease often progresses atypically. Parents need to be extremely attentive to the condition and behavior of the newborn.
The initial stage of epilepsy in children under one year of age is characterized by the following signs:
- sudden fading;
- cessation of swallowing movements;
- throwing back the head;
- trembling eyelids;
- an empty, seeing nothing look;
- complete contactlessness.
After this, loss of consciousness and convulsions occur, not always accompanied by spontaneous bowel movements and urination. It should be noted that epilepsy in children under one year of age has a kind of prelude and completion. Harbingers of an attack are increased tearfulness, excessive excitability, and febrile temperature. After the seizure ends, the baby does not always fall asleep.