When is Teraligen prescribed?
Neuroleptic
Teraligen is a drug from the group of antipsychotics (neuroleptics). The main active ingredient is alimemazine tartrate. The drug is well tolerated by patients and is prescribed for mild nervous and mental disorders, since in severe disorders its effectiveness is not enough.
Teraligen is often used to treat children, adolescents and the elderly due to the low likelihood of unwanted side effects.
Teraligen is used in neurological practice to treat neuroses and neurosis-like conditions, psychosomatic diseases, and rarely to get rid of allergy symptoms due to its antihistamine properties (not recommended for motorists and people whose work involves high concentration of attention). Teraligen reduces the excitability of the nervous system and is indicated for the following patient conditions:
- senestopathy
- hypochondria
- phobia
- asthenia, psychasthenia
- anxiety or depression in diseases of somatic origin
- various sleep disorders
Most of these symptoms are included in extensive symptom complexes of mental illnesses, such as severe depressive disorder, obsessive-compulsive disorder, etc.
In addition, such conditions can be experienced by people after operations, stress, and other diseases, i.e. as a temporary, non-progressive phenomenon. Teraligen is not a treatment for the underlying disease; it only alleviates some of its symptoms. Often it is not prescribed in psychiatric practice, but is used to correct conditions that are borderline normal.
During tests and exams
Teraligen is often prescribed to teenagers, especially when preparing for exams or in difficult family situations, because... in cases of excitement and anxiety, they develop insomnia (often with nightmares), a long-term depressed state (depression) with symptoms of painful, unclear sensations throughout the body (senesthopathy). Adolescents, especially vulnerable in this condition, begin to think of their feelings as an incurable, serious illness (hypochondria), and experience an obsessive fear of death (phobia).
Sedative for pregnant women: which medications are suitable
The main factor in getting rid of these conditions is a good life situation or at least therapeutic work, but Teraligen significantly increases the effectiveness of other treatment methods.
In addition, due to the structure of the active substance, the use of Teraligen enhances the effect of other sedatives and antipsychotics.
Teraligen is not a strong antipsychotic drug, so it is not suitable for therapy during manic episodes, schizophrenia, or acute psychotic conditions. It is used to treat mentally healthy people under stress. The drug is not a narcotic and does not cause addiction or severe side effects.
Directions for use and dosage
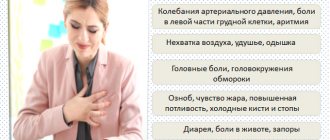
Eglonil is indicated for the treatment of vegetative-vascular dystonia with the development of the following symptoms:
- hypertensive;
- hypotonic;
- mental disorder syndrome;
- cephalgia (headaches);
- neurogastric syndrome.
The dose of Eglonil is calculated depending on the clinical picture of vegetative-vascular dystonia.
- For severe mental disorders, at least 600 mg per day is prescribed. The maximum daily dose varies from 800 to 1600 mg.
- For mild neurotic conditions, the drug is taken at 400–600 mg per day. Begin therapy with a minimum dose, then gradually increase if well tolerated.
- When treating VSD, it is preferable to use short courses of up to two weeks. If the clinical effect is good, repeat courses are prescribed with a break of at least 6 months.
- For the treatment of cephalgia with VSD, the drug is taken in a dosage of 100 to 300 mg per day. The dose is selected individually upon achievement of the expected clinical effect.
- For neurogastric dystonia syndrome, the initial dose is prescribed at 200 mg, followed by a maximum doubling.
- For therapy in childhood, the maximum daily dose is selected at the rate of 5 mg/kg of the child’s body weight.
Eglonil should be taken after meals with a small amount of water. It is advisable to divide the daily dose into two or three doses. To prevent the development of insomnia, the drug is taken two to three hours before bedtime.
Contraindications
Like all drugs that affect the nervous system, Teraligen should be used with caution in people who are alcohol dependent (since alcohol is also a psychoactive substance). In addition, Teraligen should not be taken by children under 7 years of age, pregnant or lactating women. People with problems in the urinary system should also warn their doctor about their disease when prescribing medication, because in this case, the active substance will take longer to be eliminated from the body than in a healthy person and can lead to a toxic effect.
Teraligen
Teraligen should not be taken by people with chronic muscle weakness (myasthenia gravis), Reye's syndrome, parkinsonism, or hypersensitivity to antipsychotic drugs. All these features of the body are aggravated by the use of antipsychotics due to the blocking of specific receptors. In addition, people with glaucoma should also warn their doctor about this disease, because Teraligen may cause changes in intracranial and intraocular pressure.
The main contraindications for use are children under 7 years of age, pregnancy and breastfeeding. Also, the drug should not be used by people with diseases of the excretory system (liver, kidneys) and parkinsonism, because it aggravates the course of the disease.
Interaction with other drugs
The active component of Teraligen intensifies the effect of hypnotics, opioid analgesics, tranquilizers and antipsychotics, as well as drugs for general anesthesia, m-anticholinergics and drugs for lowering blood pressure. When combining techniques, dosage adjustment is necessary.
When used simultaneously with Teraligen, amphetamine derivatives, m-cholinomimetics, ephedrine, levodopa, guanethidine, dopamine, the effect of the latter is weakened.
Concomitant use with ethyl alcohol and drugs that suppress the central nervous system results in depression of the central nervous system.
We invite you to familiarize yourself with Levomekol ointment - instructions for use, what it helps with, what it is used for?
When combining the use of Teraligen with antiepileptic drugs and barbiturates, the seizure threshold is reduced.
Combination with beta-blockers increases the concentration of the latter in the blood serum, which can provoke a decrease in blood pressure and the occurrence of arrhythmia.
In case of simultaneous use with bromocriptine, its effect is weakened, and the concentration of prolactin in the blood plasma increases.
The combination of alimemazine with tricyclic antidepressants, as well as anticholinergic medications, intensifies the m-anticholinergic properties of alimemazine.
Taking Teraligen with MAOIs and phenothiazine derivatives increases the likelihood of arterial hypertension and extrapyramidal disorders. Combined use should be avoided.
When taken with medications that inhibit bone marrow hematopoiesis, the likelihood of developing myelosuppression increases.
Alimemazine enhances the hepatotoxic properties of other drugs.
Side effects
Common side effects when using Teraligen are lethargy, increased fatigue, and the need for more sleep. However, paradoxical reactions may also occur: they are characterized, on the contrary, by psychomotor agitation, insomnia or nightmares, and anxiety. Other side effects include sensitivity to light, blurred vision, constipation, tachycardia, and problems with urination. As noted earlier, side effects are quite rare when using this drug.
With an overdose of the drug, the same reactions occur as with side effects, only in a more intense form. The patient may experience a state of depressed consciousness – i.e. react slowly and weakly to external stimuli, speak rarely and little, rarely his condition can be close to comatose.
To avoid toxic effects, you should not drink alcohol during treatment with Teraligen. Also, this drug is incompatible with MAO inhibitor drugs: during joint use, the patient’s blood pressure may sharply decrease and extrapyramidal disorders (convulsions, paralysis) may occur.
Fucicort cream: reviews, principle of action and other useful information
During treatment, liver function should be monitored and a general blood test should be taken regularly. During the period of admission, you should refrain from driving vehicles and work that requires high concentration.
Patient reviews
Doctors say that you should not take the drug Teraligen on your own. Reviews and user forums indicate conflicting effects of treatment. In some patients, after just a few days, sleep is restored, irritability decreases, and inexplicable fears and anxiety disappear.
However, many people feel dizzy and lethargic while working. In some people, no therapeutic effect was observed at all, and only side symptoms occurred (overexcitement). In the treatment of depression and phobia, the medicine has established itself as a good “helper” in complex therapy.
Note that there are much more positive reviews about the drug than negative ones. But it is worth considering that the medicine is a complex antipsychotic, and its uncontrolled use can cause serious complications, so be sure to consult a doctor before taking it.
Mechanism of action
The active substance in Teraligen, a derivative of alimemazine, blocks dopamine receptors. Dopamine is a neurotransmitter that transmits excitation from one nerve cell to another. By reducing the perception of dopamine by specific receptors, Teraligen's composition slows down and makes mental processes in general less intense. In a state of increased anxiety, the patient is in constant nervous tension, which depletes his brain cells and in turn increases the negative effects (nightmares, fears, irritability).
The action of Teraligen by reducing the activity of nerve cells makes it possible to restore their resources and normalize the functioning of the psyche.
Dopamine receptors in various parts of the brain not only transmit information about mental processes. Teraligen, by blocking receptors in various parts of the brain, in addition to sedative, also has antiemetic, antitussive and hypothermic effects. At the same time, it acts quite quickly - the onset of the effect occurs within 15-20 minutes, and the duration of action lasts for 6-8 hours.
Synonyms of nosological groups
| Category ICD-10 | Synonyms of diseases according to ICD-10 |
| F06.6 Organic emotionally labile [asthenic] disorder | Asthenic disorders |
| Asthenic conditions | |
| Asthenic disorder | |
| Asthenic disorder | |
| Asthenic condition | |
| Asthenic phenomenon | |
| Astheno-vegetative disorder | |
| Astheno-depressive disorder | |
| Astheno-neurotic condition | |
| Asthenodepressive disorder | |
| Asthenodepressive state | |
| Asthenohypochondriacal phenomena | |
| Asthenoneurotic disorder | |
| Hypochondriacal and asthenohypochondriacal condition | |
| Organic asthenodepressive disorder | |
| Psychoasthenia-like disorder | |
| F40 Phobic anxiety disorders | Obsessive fears |
| Anxiety neurosis | |
| Anxiety neurosis | |
| Night terrors | |
| Acute anxiety disorder | |
| Paroxysmal fear syndrome | |
| State of fear | |
| Fear | |
| Phobias | |
| Phobic disorders | |
| Phobia | |
| Feeling of fear | |
| F41.1 Generalized anxiety disorder | Generalized anxiety |
| Generalized anxiety disorders | |
| Anxious reaction | |
| Anxiety neurosis | |
| Phobic neurosis | |
| F41.2 Mixed anxiety and depressive disorder | Depression with anxiety-depressive components |
| Mixed anxiety and depression | |
| Anxious depression | |
| Anxious-depressive mood | |
| Anxiety and depression | |
| Anxiety and depression | |
| Anxiety-depressive syndrome | |
| Anxiety-neurotic conditions | |
| F44 Dissociative [conversion] disorders | Dissociative phenomena |
| Conversion disorders | |
| Conversion symptoms | |
| Pseudo-dementia | |
| Psychogenic psychosis | |
| F45 Somatoform disorders | Psychosomatic diseases |
| Psychosomatic disorders | |
| Psychosomatic disorder | |
| State of agitation in somatic diseases | |
| Functional psychosomatic disorders of the cardiovascular system | |
| F45.2 Hypochondriacal disorder | Asthenohypochondriacal phenomena |
| Hypochondriacal-senestopathic syndrome | |
| Hypochondriacal disorders | |
| Hypochondriacal neurosis | |
| Hypochondriacal and asthenohypochondriacal condition | |
| Hypochondria | |
| Senesto-hypochondriacal disorders | |
| Senesto-hypochondriacal disorders | |
| F45.3 Somatoform dysfunction of the autonomic nervous system | Cardioneurosis |
| Cardiovascular neurosis | |
| Neurocirculatory dystonia syndrome | |
| Somatovegetative disorder | |
| Somatovegetative complications | |
| F48 Other neurotic disorders | Neurosis |
| Neurological diseases | |
| Neurotic disorders | |
| Neurotic state | |
| Psychoneurosis | |
| Anxiety-neurotic conditions | |
| Chronic neurotic disorders | |
| Emotional reactive disorders | |
| G47.0 Disturbances in falling asleep and maintaining sleep [insomnia] | Insomnia |
| Insomnia, especially difficulty falling asleep | |
| Desynchronosis | |
| Long-term sleep disturbance | |
| Difficulty falling asleep | |
| Difficulty falling asleep | |
| Difficulty falling asleep | |
| Insomnia | |
| Short-term and transient sleep disturbances | |
| Short-term and chronic sleep disorders | |
| Short or shallow sleep | |
| Sleep disturbance | |
| Sleep disturbance, especially during the falling asleep phase | |
| Sleep disorders | |
| Sleep disorders | |
| Neurotic sleep disorder | |
| Shallow, shallow sleep | |
| Shallow sleep | |
| Poor sleep quality | |
| Night awakening | |
| Night awakenings | |
| Sleep pathology | |
| Post-somnia disorder | |
| Transient insomnia | |
| Problems falling asleep | |
| Early awakening | |
| Early morning awakening | |
| Early awakenings | |
| Sleep disorder | |
| Sleep disorder | |
| Persistent insomnia | |
| Difficulty falling asleep | |
| Difficulty falling asleep | |
| Difficulty falling asleep in children | |
| Difficulty falling asleep | |
| Difficulty falling asleep | |
| Persistent insomnia | |
| Deterioration of sleep | |
| Chronic insomnia | |
| Frequent night and/or early morning awakenings | |
| Frequent awakenings at night and a feeling of shallow sleep | |
| R45.1 Restlessness and agitation | Agitation |
| Anxiety | |
| Explosive excitability | |
| Internal excitement | |
| Excitability | |
| Excitation | |
| Excitement is acute | |
| Psychomotor agitation | |
| Hyperexcitability | |
| Motor excitement | |
| Relief of psychomotor agitation | |
| Nervous excitement | |
| Restlessness | |
| Night restlessness | |
| Acute stage of schizophrenia with agitation | |
| Acute mental agitation | |
| Paroxysm of excitement | |
| Overexcitement | |
| Increased excitability | |
| Increased nervous excitability | |
| Increased emotional and cardiac excitability | |
| Increased arousal | |
| Mental excitement | |
| Psychomotor agitation | |
| Psychomotor agitation | |
| Psychomotor agitation | |
| Psychomotor agitation in psychosis | |
| Psychomotor agitation of an epileptic nature | |
| Psychomotor paroxysm | |
| Psychomotor seizure | |
| Symptoms of arousal | |
| Symptoms of psychomotor agitation | |
| State of agitation | |
| State of anxiety | |
| State of excitement | |
| A state of heightened anxiety | |
| State of psychomotor agitation | |
| States of anxiety | |
| States of arousal | |
| State of agitation in somatic diseases | |
| State of excitement | |
| Feeling restless | |
| Emotional excitement |
The medicine can be stored for 3 years in a dry and cool place. It is very important to keep the tablets away from children and direct sunlight.
Important instructions
If the patient undergoes long-term treatment, it is necessary to constantly conduct blood tests to ensure normal liver function. If you neglect such an event, serious consequences for a person may occur. Experts say that this is a review confirmed by experience. Teraligen may cause riboflavin deficiency when taken for a long time. Therefore, it is necessary to take additional microelements. Due to increased prolactin, false positive pregnancy results are possible. If skin rashes occur, it is worth determining whether they appeared due to the drug. To do this, the tablets are discontinued 72 hours before the study. Alcohol during therapy can cause serious problems such as disorientation, respiratory depression, blindness, and in some cases even cardiac arrest.