From this article you will learn:
- Why insomnia may occur with dementia
- What medications will help against insomnia in dementia?
- Can folk remedies relieve insomnia in dementia?
Insomnia is one of the characteristic manifestations of a disease such as dementia. It appears in the form of a reduction in sleep time at night, frequent awakenings after falling asleep, wandering at night, waking up early, and sleeping too long during the day. These symptoms create difficulties for people caring for an older person or simply living with them. If insomnia is diagnosed with dementia, what should be done to alleviate the patient’s condition? We'll talk about this in our article.
Symptoms
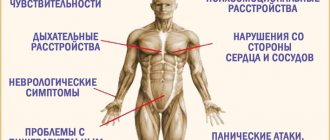
Experts identify three main groups of symptoms characteristic of chronic insomnia:
- Post-somnia. Premature or early awakening, within 2-3 hours after which there is a lack of satisfaction with sleep, a feeling of fatigue, and causeless apathy.
- Presomnic. This group combines symptoms related to the process of falling asleep. A person’s inability to fall asleep for 1 or more hours, the occurrence of negative thoughts, difficulty finding a comfortable body position, interruption of sleep even by small noises indicate presomnia disorders.
- Intrasomnic. The patient often wakes up during the night, and even minor factors of both internal (nightmares, discomfort) and external (sounds, smells) origin can wake him up. At the same time, it can be difficult for a person to fall asleep again.
As a result, the patient's memory and attention may deteriorate significantly, and he will feel tired. There are frequent complaints of excessive sleepiness during the day, anxiety disorders, and pain may appear.
Can't sleep? Listen, watch, read
If you suffer from insomnia, listen to the following recommendations: - Don't go to bed or try to fall asleep if you don't want to sleep. Try not to sleep during the day, even when you want to. Don't go to bed too early. Follow your diet. Do not overeat before going to bed, after 18:00 do not drink tonic drinks (hot chocolate, coffee, tea). Play sports at least 2-3 times a week and do gymnastics every morning or during the day, avoid intense exercise before bed. Walking or cycling before bed can be relaxing. — The bedroom is not a place for stress and conflicts, do not go to bed irritated. Try to relax at night - water treatments, light massage, meditation, an interesting (but not exciting) book are good for this. — Develop rules for getting ready for bed and follow them. Train yourself to go to bed at the same time. If you can't sleep, read a little or listen to soft music. Create comfortable conditions in the bedroom: ventilate the room before going to bed, eliminate extraneous sounds if they bother you, if the air in the bedroom is too dry, install a humidifier in it. Attention! Never take alcohol as a sleep aid, although many may recommend it in small doses. Indeed, in some cases, alcohol helps to fall asleep better, but this is an apparent improvement: sleep becomes shallow (superficial), fragmented, often short; the aftereffect of alcohol can cause morning headaches, fatigue, decreased performance during the day, which, in turn, aggravates insomnia.
Forms
Depending on the causes of chronic insomnia, there are two main forms of this disorder.
Primary
In this case, specialists often have difficulty identifying the factors leading to the development of long-term sleep disorders.
It, in turn, is divided into three subspecies.
Pseudo-insomnia
In this case, a distortion of the subjective perception of sleep duration occurs. In fact, it is 6 or more hours, but for some reason the patient forgets most of the periods of sleep, and he has the erroneous belief that they are extremely small and do not satisfy his needs for night rest.
Adaptive subspecies
The most common, has an average duration of three months. It occurs due to excessive nervous excitement caused by depression, stressful situations or strong emotional experiences.
Psychophysiological subtype
It can develop if the patient suffers from a sleep disorder for a long time, as a result of which psychological disorders are added to it. A person develops a fear associated with the process of falling asleep. This leads to the fact that when trying to fall asleep, the patient involuntarily brings his nervous system into an excited state, most often with a large number of active body movements.
Secondary
This form has a direct connection with pathologies of a psychoneurological nature. A significant proportion of patients (about 70%) suffering from depression or neurosis suffer from insomnia. Liver diseases, kidney pathologies, diabetes mellitus, arterial hypertension can also cause the development of insomnia.
Depending on the severity of the patient's condition, insomnia is divided into three types.
Easy
The occupational and or social functioning of a person suffering from insufficient sleep duration or depth is only slightly impaired. At the same time, feelings of fatigue, weakness, anxiety and irritability during the daytime often occur, but not always.
Moderate
Deterioration in general health, drowsiness, weakness and anxiety during the day are constantly present. The patient's ability to adequately function professionally and socially is moderately reduced.
Heavy
This is a significant deterioration in the patient’s quality of life and well-being, resulting from chronic insomnia.
Depending on the individual characteristics of the body, both the deterioration of the patient’s condition who does not receive qualified care and its stabilization are possible. However, regardless of the form of the disease, one should not expect that the problem will solve itself, without outside intervention.
“Please go away, insomnia...”
Surely each of us has suffered from insomnia at least once in our lives. Perhaps it happened the night before an exam or before an important meeting, when you were trying to go to bed early and get a good night's sleep. But instead, they lay awake for hours, painfully scrolling through the options for upcoming events. Or, having come after a hard day at work, literally “falling asleep on the go,” you went to bed dreaming of the desired rest, but, alas, the bed is uncomfortable, or some barely audible sounds are disturbing you, and the desire to sleep disappears irrevocably. Such problems regularly occur in 30-45% of people, and in half of them they become chronic; about 80% of patients complaining of poor sleep suffer from neuroses.
Reasons for appearance
There are a number of reasons that can lead to the development of a chronic sleep disorder in a person. Moreover, even a competent specialist is not always able to quickly and correctly identify them in each specific case.
The most common are the following:
- Bad habits. This category includes smoking, alcoholism, drug addiction, and in some cases overeating.
- Taking certain medications (in particular, psychotropic drugs).
- Mental disorders (anxiety and depression, Parkinson's disease).
- Chronic pain of various origins.
- The rhythm of life and or the patient’s daily routine. In particular, sleep disturbances are often observed in people who work shifts and are forced to regularly fly between time zones. Insomnia is also often experienced by those who watch movies or television programs for a long time, or work or play on the computer at night.
- Pathological conditions of internal organs, as well as the endocrine system.
- Apnea – both central and obstructive. In both the first and second cases, the cause of sleep disturbance is respiratory arrest.
- Post-traumatic syndromes, psychological trauma.
- Pathologies associated with the brain .
- Climax.
Regardless of the causes of insomnia, it is almost impossible to cope with the disease without the help of specialists, and in some cases, attempts at self-medication can pose a danger to the patient. Insomnia, especially if it is chronic, not only significantly worsens the quality of life, but also has a negative impact on a person’s health.
In men
The danger of insomnia for the stronger sex lies in endocrine imbalance; against the background of insomnia, men experience a decrease in the production of sex hormones. As a result, libido and potency decrease, and the process of ejaculation during intimacy accelerates.
During the daytime, they feel overwhelmed, experience discomfort when driving vehicles (they cannot concentrate, are poorly oriented in space, lose the sharpness of their reactions), men often lash out at others, experiencing increased nervousness and irritability.
Insomnia is extremely dangerous for men suffering from cardiovascular diseases; the inability to replenish vital resources during sleep provokes an exacerbation of coronary disease and the occurrence of heart attacks.
Male insomnia is often caused by:
- strenuous night work;
- alcohol and tobacco abuse.
Diagnostics
A thorough assessment of the patient's condition must be carried out by a physician during the diagnosis process. This is due, in particular, to the fact that insomnia can be a symptom of a number of serious pathologies.
On this topic
- Sleep disorders
13 foods you can eat in the evening to improve your sleep quality
- Natalia Sergeevna Pershina
- March 29, 2020
The following signs should attract special caution and close attention of a specialist:
- the appearance of pain, deterioration of attention and or memory;
- depressive episodes: minor or major;
- the patient develops a persistent general anxiety that has no objective connection with real situations or objects;
- complaints of severe fatigue or drowsiness during the day.
When assessing primary insomnia, the clinician usually relies on medical history. If it is carried out correctly, then this makes it possible to correctly describe not only the disorder itself (including its severity, duration and variations), but also to take into account the consequences that occur during the daytime.
It is important to find out whether the patient is taking any medications, since some groups of them can cause sleep disorders.
Keeping a sleep diary is recommended. In most cases, the patient himself makes entries in it, however, in some cases it is permissible to delegate this responsibility to a close relative. Such a diary helps the specialist in the process of assessing the severity of the patient’s condition and makes it possible to determine how variable insomnia is.
In addition, the patient may have bad habits that can negatively affect the quantitative and qualitative characteristics of sleep. An example would be a person staying in bed for a long time (8 hours or more), as well as napping. During the treatment process, the diary becomes a source of information about the patient's reaction to the procedures.
In order to objectively assess the amount of sleep, in most cases the polysomnography method is used.
The following diagnostic measures are also required:
- To assess somatic pathologies, a general physical examination should be performed.
- Detection of apnea, narcolepsy, periodic involuntary movements during sleep.
- Laboratory diagnostics of the patient’s biological material to exclude the presence of thyroid pathologies, restless legs syndrome caused by vitamin B12 deficiency, as well as iron deficiency anemia.
- Sleepiness assessment using the Ashworth scale.
The last type of diagnosis is carried out, among other things, to determine the subjective level of daytime sleepiness, and is based on a scoring system for assessing the patient’s condition under certain conditions.
Neuroleptic (antipsychotic) Teraligen - review
Life is not always a simple thing, or rather, not simple at all, and everyone has internal crises. A year ago, I had a similar crisis, neurotic insomnia began.
At that time, I knew little about the nature of this neurotic symptom and suffered greatly, did not sleep, and suffered from panic attacks at night.
As a result, I ended up seeing a psychiatrist, who prescribed me this drug.
So, in what cases is it used?
Indications for use:
neuroses and neurosis-like conditions of endogenous and organic origin with a predominance of senestopathic, hypochondriacal, phobic and psychovegetative disorders;
psychopathy with asthenic and psychoasthenic disorders;
anxiety-depressive conditions within the framework of borderline and vascular diseases;
senestopathic depression;
somatized mental disorders;
states of excitement and anxiety in somatic diseases;
sleep disorders of various origins;
allergic reactions (symptomatic treatment).
Yeah, that's right. Insomnia in most cases is of a neurotic nature , as it was for me.
What is neurosis and how does it arise? In everyday language, a combination of the following factors leads to neurosis: 1) predisposition (impressionable character, increased emotionality and suspiciousness) 2) upbringing and childhood events leading to the development of a neurotic perception of the world, sometimes carrying hidden internal psychotraumas 3) a series of psychologically traumatic factors, gradually , but naturally hitting the “most sacred” inside a person, his sore spots (and the person does not always realize the extent to which this actually traumatizes him). In other words, neurotic symptoms appear like this: things seemed to be going mediocre, then there was trouble here, then there, it seemed like no catastrophes happened right here and now (although they could have happened in the past), the person was just depressed, and then hop - and agoraphobia or cardiophobia , or – oh my God – insomnia.
Of course, people immediately get scared, run with their symptom to doctors and psychotherapists, as was the case with me, and begin to try to treat this symptom. In my case, I rushed to treat insomnia.
In other words, I developed a fear of insomnia and it was because of it that I did not sleep. I tried my best to fall asleep, I couldn’t because I was too tense and scared (naturally), I was even more scared and... nothing good.
What was the drug supposed to do?
Pharmacodynamics:
Antipsychotic drug (neuroleptic), has antihistamine, antispasmodic, serotonin-blocking and moderate α-adrenergic blocking effects, as well as antiemetic, hypnotic, sedative and antitussive effects.
The antipsychotic effect is due to the blockade of dopamine D2 receptors of the mesolimbic and mesocortical systems.
The sedative effect is due to the blockade of adrenergic receptors in the reticular formation of the brain stem; antiemetic effect - blockade of D2 receptors of the trigger zone of the vomiting center; hypothermic effect - blockade of dopamine receptors of the hypothalamus. The onset of the effect is after 15–20 minutes, the duration of action is 6–8 hours.
It has low antipsychotic activity, therefore it is ineffective in acute psychotic conditions.
In other words, the drug “turns off” tension in the brain. Oh yes, this is NOT a sleeping pill . It is not intended to put you to sleep, it is simply meant to turn off anxiety and put the person into a state of complete indifference. Therefore, it is prescribed not only in cases of insomnia.
The drug is quite strong, so initially a quarter to a half of a tablet is prescribed. I didn’t fall asleep quickly, but it really did “turn off” my brain. Gradually I increased the dose to one tablet.
My mistakes
My mistake (or rather, as I believe, the mistake of a psychiatrist) was that we did not eliminate those internal conflicts that led to neurosis, but tried to extinguish the insomnia itself. Therefore, just as I was afraid of her, I continued to be afraid, remaining unable to get out of the vicious circle of my fear.
The worst thing : gradually, subconsciously, I stopped believing that I was able to fall asleep on my own, because only pills helped me with this. Again, insomnia is NOT an organic disorder, it is only the result of our own beliefs. As a result, I needed more and more pills.
At the end (a month and a half later) I pulled myself together and realized that the drug would not solve my problem.
Yes, it helps you “pass out” and fall asleep, it turns off your brain, but it still won’t find a way out of your problems.
It is worth noting that the drug is sold strictly according to a prescription, and you cannot simply buy it. Not compatible with all drugs, and absolutely not compatible with alcohol. TO
In addition, I experienced a SIDE EFFECT: with long-term use, ALL psychotropic drugs have the ability to disrupt hormonal levels. In my case, I experienced a significant increase in prolactin, which is not good. If you have problems with hormones, you should definitely inform your doctor and it is advisable to consult with an endocrinologist.
Cancellation effect
Yes, it was, and quite strong. This was partly my fault, since I canceled the appointment abruptly. The withdrawal effect occurred after five to six days (since the drug tends to accumulate in the body) and was expressed in a significant increase in anxiety with panic attacks.
Besides this, another minus is a severe hangover in the morning. After my first use of the drug, I had to sit at home almost the entire day; I had terrible drowsiness and weakness.
Total: yes, the drug performs the stated actions, but it will not be a solution to your problems if there are no organic disorders at the root of it (since the drug is used for them too).
I give it a three, since the drug is still quite heavy and using it for neurosis is fraught with psychological addiction, as well as possible hormonal imbalance. In addition, the withdrawal effect in my case was strong and very unpleasant.
From my own experience, I can tell you that if you are also faced with the problem of insomnia, this is a reversible disorder, and first of all you need non-medicinal help. The key to successfully exiting such a state is solving your true internal problems.
If you have to experience this state now, I am with you, I understand you, I empathize with you. I went through all this myself. There is a way out, and it doesn’t come in pills. In my case, I was helped by people who simply changed my life, but that's another story.
Source: https://irecommend.ru/content/primenenie-pri-nevroticheskoi-bessonnitse-prichiny-ustranenie-oshibki-podrobnyi-otzyv-s-reko
Treatment
Once a patient has been diagnosed with chronic insomnia, the doctor develops an individual treatment strategy based on a number of factors, including the causes of the disease and the severity of the condition. In general, the essence of therapy is to relieve the problems that cause insomnia, both physiological and somatic.
Expert research confirms that a combination treatment approach, including behavioral interventions in combination with pharmacological drugs, is more effective than the use of individual types of therapy.
Pharmacological treatment is considered acceptable to alleviate the condition of patients suffering from short-term insomnia. In cases where the patient has persistent insomnia, pharmacotherapy can only be used in combination with behavioral strategies. Experts distinguish two lines of influence through the use of medications.
First
It has high levels of efficiency and safety. The medications used in this case, in turn, are divided into two main groups.
Benzodiazepines
They help increase the total duration of sleep, reduce the number of night awakenings, and also significantly reduce the time it takes to fall asleep. Patients who have been diagnosed with apnea or chronic pulmonary failure should use drugs in this group with caution.
Contraindicated for pregnant women, elderly people suffering from liver dysfunction, as well as patients with a history of using psychoactive substances in large quantities.
Non-benzodiazepine hypnotics
Most often, patients are recommended to take drugs from this group, such as Zopiclone or Zolpidem.
Second
This line includes antihistamines (they are sleeping pills that can be purchased at pharmacies without a prescription), as well as tricyclic antidepressants. In this case, the level of tolerability, as well as the effectiveness of pharmacological agents, is characterized as moderate.
On this topic
- Sleep disorders
All about sleep paralysis
- Natalia Sergeevna Pershina
- March 26, 2020
Among the non-pharmacological treatment strategies for insomnia, the most effective are the following:
- therapy ;
- relaxation techniques;
- behavioral interventions;
- teaching the patient hygiene ;
- stimulus control
- restriction ;
- cognitive interventions;
- method of paradoxical intentions.
Depending on the individual characteristics of the patient’s body, as well as the causes of the sleep disorder, either one strategy of such influence or a complex of them can be used. If the treatment is organized correctly and the patient strictly follows all instructions, in the vast majority of cases the problem can be successfully solved.
Insomnia with dementia: what to do and how to help
There is no standard, template method for treating insomnia in dementia.
Each case is considered by specialists individually. This is primarily due to a large number of pathogenetic mechanisms preceding the disease. With dementia, patients often experience emotional disturbances. Therefore, in cases of severe depressive moods, antidepressants are prescribed. The duration of therapy is directly affected by the severity of the pessimistic state. In most cases, it lasts about six months, since antidepressants produce a cumulative effect, and the first positive changes are observed a few weeks after starting treatment. Nootropic drugs are used as mandatory drugs for the treatment of insomnia in dementia of any type. They help improve cognitive performance and are effective for memory recovery. In addition, modern drug therapy often uses tranquilizers to relieve anxiety and fear.
Recommended articles to read:
- Social services for older people
- Diseases of old age
- Valuable tips on how to choose a boarding house
In case of senile dementia, the patient should be provided with regular intake of sedatives, sedatives, hypnotics, and medications that improve blood circulation in the brain and slow down the breakdown of cells. For example, very often doctors prescribe Phenozepam, which relieves symptoms of insomnia, anxiety and other psychotic conditions. Dementia should not be treated at home for any severity or type of disease. The selection of drugs should be carried out only by a doctor, which will eliminate the possibility of developing undesirable effects. Patients are strongly discouraged from taking medications that reduce concentration and also negatively affect memory.
Read material on the topic: Health of older people
Prevention
A number of preventive measures can help prevent the occurrence of sleep disorders, including:
- formation and adherence to routine ;
- moderate regular physical activity;
- balanced and moderate nutrition;
- maintaining hygiene ;
- minimizing emotional experiences in the evening.
If symptoms of insomnia occur, you should seek help from qualified professionals. Solving sleep problems becomes more difficult over time, as the disease can become chronic.
Recommendations for drugs
Below you will see a list of recommended drugs and their characteristics.
Tizercin
Antipsychotic drug (neuroleptic) of the phenothiazine series.
Pros: calms, has a slight analgesic effect.
Cons: increases pain threshold, lowers blood pressure
Contraindications: antihypertensive drugs are incompatible with Tizercin.
Price: 214 rub.
Analogs: Sonapax, Aminazine, Neuleptil
Reviews: according to reviews, the drug is quite effective, but causes lethargy.
Teraligen
The chemical structure of the drug is similar to the formula of diprazine and levomepromazine; the drug blocks serotonin and has a strong sedative effect.
Pros: Induces sleep in no time.
Cons: many people feel very tired and groggy during the day.
Contraindications: the drug has a lot of contraindications and should be taken after consultation with your doctor.
Price: 548 rub.
Analogues: Diprazin, Pipolfen.
Reviews: according to reviews, the drug is quite effective, but has certain consequences in which a severe state of lethargy and weakness is felt in the first 5-6 hours after waking up.
Sonapax
The drug has an active substance based on phenothiazine and has an effect on the central and peripheral nervous system.
Pros: the drug helps you fall asleep quickly, balance and calmness, and also relieves anxiety during the day.
Cons: in some patients it causes a sharp drop in blood pressure to critical levels.
Contraindications: the drug should not be used for depression.
Price: 350 rub.
Analogues: Tizercin, Aminazine, Neuleptil.
Reviews: the drug is quite effective, but in many patients it causes a state of excessive calm, associated with a decrease in mental activity.
Aminazine
The medicine is a phenothiazine derivative, a powerful tranquilizer.
Pros: Aminazine is the most budget-friendly option for antipsychotic drugs.
Cons: significantly depresses the psyche, leads to a lethargic state, aggravates depression.
Contraindications: for neuroses and personality disorders.
Price: 155 rub.
Analogues: Aminazine, Thorazine.
Reviews: psychiatrists working in psychiatric clinics speak of the drug as a last resort, used to quickly and effectively relieve agitation in violent patients.
Neuleptil
A phenothiazinine derivative with moderate antipsychotic and sedative effects.
Pros: selectively normalizes behavior, has a good hypnotic effect.
Cons: respiratory and central nervous system depression.
Contraindications: if you have diseases of the cardiovascular system, the drug should not be taken.
Price: 637 rub.
Analogues: Thiodazine, Sonapax.
Reviews: enhances the effect of sleeping pills, has a mild but fairly stable sedative effect.
These remedies are the most common and are prescribed for sleep. You can choose any of them, but you must first consult with your doctor, as medications have a number of common side effects:
- strange feeling of tension and restlessness (akathisia);
- Parkinson's tremor and movement abnormalities;
- weight gain;
- high blood sugar;
- new or worsening diabetes;
- and rare cases of cardiac arrhythmia, which can cause sudden death.
The presented drugs contain the active ingredient phenothiazine and have a similar principle of action. Phenothiazine drugs block the action of dopamine in the brain, but their exact mechanism of action is unknown.
Phenothiazine antipsychotics are used in the treatment of psychotic symptoms associated with schizophrenia or bipolar disorder. Some phenothiazines (such as prochlorperazine and chlorpromazine) are also effective in relieving other symptoms not associated with psychosis, such as nausea, vomiting, prolonged hiccups, tetanus symptoms, and hyperexcitable behavior in children.