4% of people over 80 suffer from Parkinson's disease, 47% of the 85+ age group are diagnosed with Alzheimer's disease. What is the difference between these serious illnesses?
Neurological diseases become more and more common among people as they age. However, it is worth remembering that not all of them lead to complete personality disorder and memory loss. Among them, two prominent diseases today are Parkinson’s disease and Alzheimer’s disease. Many people often do not understand the difference between them. At the same time, these pathologies today often come to the fore in terms of the number of deaths.
How does Alzheimer's disease differ from Parkinson's disease?
The symptoms of the diseases are similar, and this greatly complicates the diagnosis. In the first stages, sometimes even a neurologist cannot distinguish them, so special studies are required. But the clinical picture is so unclear that neither the patient nor those around him even think about the development of the disease and do not go to the clinic. They explain all the symptoms by mental stress, stress, overwork, and pre-existing diseases.
Parkinson's and Alzheimer's disease have the same symptoms:
- Severe symptoms usually begin to appear after age 55.
- Pathologies progress slowly.
- Chronic.
- Similar initial symptoms: migraine, decreased attention, fatigue, dizziness, poor coordination of movements.
- Poor prognosis. Neither one nor the other pathology can be completely cured.
- Genetic predisposition. This is not the only reason, but it significantly increases the likelihood of developing the disease.
The biomechanisms of progression of degenerative processes are different. The causes of illnesses are being investigated, and there are several scientific theories. With all this, doctors note risk factors. Their influence provokes the launch of negative reactions in the brain and leads to structural changes.
The main differences between the diseases become clear with a qualified assessment of the clinical picture. An experienced specialist in the primary stages, having examined and questioned the patient, conducting several psychological tests, can assume the presence of one of the pathologies.
How is Alzheimer's disease different from Parkinson's disease? To answer this question, it is necessary to consider the features of the clinical picture of each disease. In Parkinson's disease you can observe:
- Stiffness of movements.
- Involuntary trembling of the limbs (tremor). In the first stages, it usually spreads only to one upper limb, then to the other, and then to the lower limbs and head.
- Sudden changes in blood pressure. They occur when a person changes body positions.
- Increased muscle tone. Over time, this provokes a change in posture. The patient moves by leaning forward, lowering his head and bending his elbows.
- Additional symptoms include increased sweating, salivation, insomnia, enuresis, and decreased sense of smell.
In this case, the patient remains in a clear consciousness. Attention and memory do not deteriorate, the level of intelligence does not decrease. That is why in Parkinson’s it is impossible to use a method that is very effective in Alzheimer’s syndrome – active mental activity. In people who have intelligence, take an active position in life, are fond of reading, analytics, and have their own hobbies, multiple chains of interneuron connections are formed in the structure of the brain.
If one of the segments of brain cells is damaged, neighboring ones take over its functions. This may reduce the risk of Alzheimer's syndrome, but does not in any way protect against Parkinson's disease.
Alzheimer's syndrome manifests itself in the form of symptoms:
- In the first stages, the patient’s condition changes little; all signs are attributed to overwork. Lethargy and apathy appear. A person thinks for a long time about the information received, analyzes it poorly and quickly forgets.
- Then memory problems become more serious, the patient often uses notes, stickers, and diaries so as not to forget anything important. Visual and auditory perception deteriorates, vocabulary decreases, and a person cannot formulate his thoughts.
- Coordination is impaired.
- Over time, a decline in intelligence becomes obvious. The patient forgets the names of objects and does not remember the meanings of words. Long-term memory is impaired, so a person recognizes with difficulty or cannot remember loved ones and acquaintances at all.
- Unmotivated aggression, irritability, and tearfulness appear. The patient cannot take care of himself independently.
- In the final stages, control over your body and its physiological functions is completely lost. The patient does not walk, does not talk, does not perceive the surrounding reality.
Both pathologies also have some common symptoms. Both diseases are accompanied by nervous disorders and depression. In the early stages, the patient loses interest in work, usual activities, and close people. Over time, deep apathy may set in, accompanied by constant anxiety and irritability.
Survival prognosis
Despite the significant differences between the diseases, the prognosis in both cases is unfavorable. There is no cure for these pathologies that can completely stop the degenerative process. Existing medications and other approaches only slow down the speed of its spread, prolonging the patient’s life and increasing its quality. On average, people with Alzheimer's disease live 7-9 years after diagnosis, subject to specialized therapy. With Parkinson's, with an adequate approach, patients live about 15 years, but at the same time their performance decreases noticeably after 8-10 years from the moment of diagnosis.
Knowing the difference between Parkinson's disease and Alzheimer's syndrome can help people notice warning signs early. The main thing is not to try to cope with them on your own, but to immediately contact a neurologist. Timely initiation of therapy against such a background becomes the key to the most favorable prognosis.
How is dementia different from Alzheimer's disease?
Patients and their loved ones are often interested in the question of how Alzheimer's disease differs from senile dementia. The latter disease can be defined as a pathology as a result of which the degenerative process of the brain begins (this is also typical for Alzheimer's syndrome).
Patients experience delays in the perception and analysis of information
ations, control over emotions decreases, memory deteriorates. Symptoms clearly manifest themselves in patients 65 years of age and older; under the influence of certain reasons, they can be observed earlier.
The difference between Alzheimer's disease and dementia is that Alzheimer's disease ends in dementia in any case. It is not always caused by Alzheimer's syndrome, since there are many other reasons that lead to the development of the disease.
Main differences:
- Alzheimer's syndrome is not accompanied by hallucinations and insomnia (in the early stages). In Lewy body dementia, all of these symptoms can appear quite early. These include impaired coordination and motor function, and temporary memory loss. The patient may not remember or recognize his loved ones one day, but the next day he may call them by name, remember everyone’s birthday, etc. With Alzheimer's syndrome, a person loses memory gradually, and in the last stages completely loses it.
- Dementia with Lewy bodies most often affects men, and Alzheimer's affects women.
- Dementia can be triggered by factors such as stroke, malnutrition, thyroid pathologies, and severe infections. Alzheimer's syndrome is caused by proteins and beta amyloid plaques that damage the brain neurons responsible for thinking and memory.
Alzheimer's syndrome and senile dementia are closely related. The main task of a specialist is to distinguish them from other lesions of the nervous system that follow a similar scenario.
Etiology
To compare Parkinson's and Alzheimer's diseases, it is necessary to understand the mechanism of their occurrence and the principle of development. Both pathologies are neurological in nature – the victim’s brain is affected. Diseases in the vast majority of cases are registered in older people. They have a chronic course, characterized by slow progression with a gradual increase in the clinical picture.
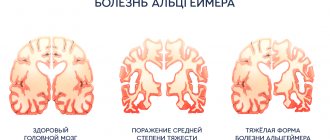
Parkinson's and Alzheimer's occur against the background of degenerative processes in the tissues of the central nervous system. This leads to the death of cell colonies, atrophy of entire areas of the brain, and a decrease in the functionality of the organ. In Parkinson's, the death of neurons responsible for the synthesis of the neurotransmitter dopamine is recorded. A deficiency of the chemical compound contributes to irritation of the cerebral cortex by the basal ganglia, which leads to a number of characteristic symptoms.
Alzheimer's, according to the main theories, is the result of the accumulation of neurofibrillary tangles and amyloid plaques in the brain tissue. This triggers a sequence of degenerative changes in the tissues of the central nervous system. The resulting massive death of neurons and structural damage to cell colonies appear only several years after the start of the process.
Diagnostics
Diagnosis of Alzheimer's and Parkinson's diseases begins with a visit to a neurologist. He will collect anamnesis, conduct an examination, prescribe a neuropsychological test, and interview the patient and his relatives. The preliminary diagnosis must be confirmed by the following studies:
- CT scan.
- Electrocardiogram.
- Complete analysis of cerebrospinal fluid and blood.
If necessary, additional studies will be prescribed. Once the overall picture is obtained, the specialist will make a final diagnosis and prescribe therapy.
Causes
The mechanisms of disease development are different, but the factors that aggravate degenerative processes in the brain are similar. It turns out that eliminating the influence of a number of irritants on the body simultaneously acts as a preventive measure for Alzheimer’s and Parkinson’s.
The following are the provocateurs of degenerative processes in the brain:
- traumatic brain injuries,
- harmful living and working conditions, poor ecology,
- severe migraines, chronic headaches,
- obesity,
- brain tumors,
- constant stress, experienced shock,
- bad habits,
- Irregular use of medications and inconsistent with the doctor.
In the case of Alzheimer's, several additional points apply. In particular, a low level of mental activity poses a danger to every person. Refusal to read, study foreign languages, or obtain higher education reduces the number of neural connections in the brain. Also
Prevention measures
It is recommended to start taking care of yourself as early as possible. Following some rules will help maintain health for many years.
Adhere to a healthy diet, eliminate or minimize the consumption of fatty, fried, and salty foods.
- Take vitamin complexes.
- Every day, engage in a feasible sport (swimming, skiing) or do gymnastics, walk.
- Follow the regime.
- Pay special attention to mental stress. You can learn poetry, solve crossword puzzles, read books, memorize phone numbers, master computer operation, and don’t give up learning a foreign language.
- Communicate with friends, loved ones, relatives, acquaintances. Discuss films with them, retell the contents of a book they read, formulate and express their opinions, analyze situations. Under no circumstances should you “lock yourself within four walls” alone with the TV.
- Find a favorite activity that will bring you joy - embroidery, decoupage, moderate work in the country, caring for animals.
- Have regular medical examinations.
Following these simple recommendations is one of the foundations of a fulfilling life.
It should be borne in mind that there is no treatment that can completely cure all of the above ailments. However, it is quite possible to slow down their negative manifestations, alleviate the patient’s condition and improve his quality of life. A good effect is manifested when taking nootropic drugs, vitamin complexes, and inhibitors. The main task of the patient and his relatives is to notice dangerous symptoms in time and immediately seek help from doctors.
Localization of changes
Alzheimer's disease is a neurodegenerative disease that is characterized by a decrease in memory, intelligence, and higher cortical functions (the ability to speak, coordinated actions, spatial orientation). The phenomenon is named after the German psychiatrist Alois Alzheimer who described it.
First of all, the location of the lesion is different. In dementia of the Alzheimer's type, pathological changes occur in the following parts of the brain:
- hippocampus, amygdala and in the lower parts of the temporal lobes;
- posterior temporal, parietal;
- frontal.
It is characteristic that the involvement of these structures occurs sequentially, and the frontal regions of the brain begin to participate in the later stages of the disease.
Parkinson's disease is characterized by predominant damage to the extrapyramidal system, namely the pallidal component and the substantia nigra.
Common central nervous system diseases in older people
Stroke
– a clinical syndrome that develops as a result of acute cerebrovascular accident.
The older a person gets, the higher the risk of stroke. For men, the dangerous age begins after 60 years, for women after 80.
Unfortunately, this disease is getting younger every year. According to statistics, a third of stroke patients are people of working age, and the share of young people was 11–15% of the total number of stroke patients.
It is important to know 3 signs of stroke development
- Suddenly distorted face (asymmetrical smile),
- weakness in the arm and leg,
- speech disorder
The less time passes between the stroke and the start of treatment, the higher the chances of a favorable prognosis.
Ischemic attacks
or transient cerebrovascular accident often occurs with very stroke-like symptoms. But this disease is different in that the symptoms that arise are reversible.
If you suspect an ischemic attack, you should immediately consult a doctor, because this disease is a harbinger of an upcoming stroke.
Cognitive impairment of the central nervous system in older people
Cognitive impairment most affects the higher brain functions of a person. A complex of critical disorders of memory, attention, speech and thinking is called dementia. It is important to understand that dementia itself is a syndrome, not a disease. Dementia is a consequence of pathological conditions of various origins.
Vascular dementia can occur as a result of a stroke or as a result of chronic diseases that impair the blood supply to the brain. Dementia caused solely by vascular cognitive impairment occurs in only 17% of all cases. A feature of vascular dementia is the reversibility of the process. Timely diagnosis of the disease and prescription of adequate therapy can stop the depression of brain activity.
Types of vascular dementia:
- multi-infarct dementia;
- dementia with single infarctions in areas of the brain that are strategically important for cognitive functions;
- dementia associated with damage to small-diameter arteries in the subcortical structures of the brain;
- hypoperfusion dementia;
- posthemorrhagic dementia;
- mixed vascular-atrophic dementia.
The vascular form of dementia is diagnosed based on a careful collection and study of the medical history, assessment of the patient’s cognitive functions and mental status. CT and MRI of the brain also help the doctor in determining the vascular nature of the symptoms.